Linking Depression, Diabetes and Alzheimer’s Disease

It has been known for many years that Alzheimer’s disease and depression are associated with type 2 diabetes. Good control of blood glucose may reduce the risk of developing Alzheimer’s disease and depression, while treating depression may improve metabolic control.
Decreased levels of brain-derived neurotrophic factor (BDNF) have also been implicated in the pathogenesis of Alzheimer’s disease and depression, and animal models have suggested that BDNF may play a role in insulin resistance.
So a group of scientists at The Centre of Inflammation and Metabolism, Department of Infectious Diseases at the University of Copenhagen in Denmark, decided to see whether BDNF plays a role in human glucose metabolism.
In the first study they looked at 233 people and found that BDNF was inversely associated with fasting plasma glucose, but not with insulin. In a second smaller study they did what are known as hyperglycemic and a hyperinsulinemic-euglycemic clamp studies, that allowed them to look at the relationships between BDNF, glucose and insulin. What they found was that output of BDNF from the brain was inhibited when blood glucose levels were elevated.
So it seems that low levels of BDNF accompany impaired glucose metabolism. Decreased BDNF may be a factor involved not only in dementia and depression, but also in type 2 diabetes, and it may be the missing link that explains the way in which the three conditions cluster together in epidemiological studies
This link between a chemical produced in the brain and diabetes is not altogether unexpected. The French physiologist Claude Bernard demonstrated that stimulation of the fourth ventricle of the brain caused glucose to rise, and it was later found that opiates put into this region of the brain could do the same thing.
This study reinforced the close links between metabolism and the brain, and gives us another reason for recommending that as we get older we must ensure that out glucose remains stable and that we do not become depressed.
Insulin Resistance in the Brain and What It Means for Dieters
Most people have been taught that increasing weight is the cause of insulin resistance, which in turn may cause an array of different health problems. That is only half true: insulin resistance may contribute to the development of obesity, and once we start gaining abdominal fat then that may indeed contribute to insulin resistance. So a vicious circle is established in which insulin resistance helps cause obesity, which in turn causes more insulin resistance.
Another thing that we have been taught for half a century that the brain is an insulin-insensitive tissue. What that means is that the uptake and use of glucose by the brain is not affected by circulating levels of glucose and insulin. That has always seemed a bit strange, because insulin is very important in cognition. Some experts believe that disturbances of insulin and closely related hormone – insulin like growth factor 1 (IGF-1) are involved in the pathogenesis of Alzheimer’s disease.
When someone is insulin resistant, they have high circulating levels of insulin, and an obvious question is whether these high insulin levels may interfere with the normal functions of the brain. This is not a new idea. It has been known for many years that high levels of triglycerides, that may be a marker for insulin resistance, may be associated with cognitive impairment in people with type 2 diabetes.
Now colleagues in London have found that people who have peripheral insulin resistance also have brain insulin resistance especially in two brain regions – the ventral striatum and prefrontal cortex – that are involved in appetite and reward.

It looks as if one of the reasons why people with insulin resistance become obese is that the normal link between the control of food intake and energy balance is broken.
This is yet more evidence that a simple diet will not work in the long term. If the problem is metabolic and involves damage to the mechanisms that control eating, the only way to help is to use a combined approach that deals not only with the composition of the diet, but the precise time when people should eat, and the psychological and social barriers that are left over from millions of years of evolution. I outline a comprehensive and highly successful weight management technique in Healing, Meaning and Purpose. Over the last few months I have had an enormous number of requests to expand that material into another book, and in between writing this blog, I am hard at work on completing a full account of exactly what we do to help people manage their weight.
Lithium and Brain Growth
There’s an interesting story about the way that lithium was found to be helpful to some people with bipolar disorder. It was thought that there was a link between bipolar disorder and gout, and gout is caused by an accumulation of uric acid in some joints. It just so happens that lithium is very good at getting guinea pigs to pass any excess uric acid in their urine. So in 1949 a medical scientist in Australia called John Cade tried lithium in bipolar disorder. It worked, but not because of any effect on uric acid: the lithium/uric acid connection only works in guinea pigs. But now, all these years later, it turns out that there may actually be a link between bipolar disorder and uric acid after all: uric acid levels often rise in people who are insulin resistant, and insulin resistance is a common feature of bipolar disorder.
The last few years have seen the growth of an impressive body of evidence about the effects of lithium on the brain. Lithium modulates the way in which many neurotransmitters act in the brain. That raised interesting questions, because many of the chemical transmitters do not only send messages between neurons, they may also stimulate the growth of cell processes and perhaps neurons themselves. Then it was discovered that lithium protects neurons by increasing the levels of a neuroprotective protein called Bcl-2. Then it was found to help stimulate the production of new neurons (neurogenesis) in the hippocampus.
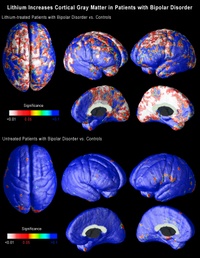
A major breakthrough came in 2000, with the demonstration that lithium increases the amount of gray matter in the human brain, probably by stimulating the production of a growth promoter called brain-derived neurotrophic factor. Gray matter is composed primarily of neurons, so this suggested that lithium was either stimulating the growth of new neurons, or causing the migration of neural stem cells, or alternatively somehow preventing the death of neurons.
Within less than two years it was confirmed that treatment with lithium increased the amount of gray matter in the brains of people with bipolar disorder.
The findings remained controversial for two reasons: first was the seeming impossibility of stimulating the production of new gray matter. That is no longer such a problem: there is more and more evidence that the adult brain can indeed produce new neurons.
The second problem was technology: the measurements were open to
different interpretations.
Now neuroscientists at UCLA, using brain scans collected by collaborators at the University of Pittsburgh School of Medicine have shown that lithium does indeed increase the amount of gray matter in the brains of patients with bipolar disorder. But what is far more important is that the effects are seen in precise regions of the brain that are thought to be implicated in bipolar disorder.
The research is published in the July issue of the journal Biological Psychiatry.
Carrie Bearden, a clinical neuropsychologist and assistant professor of psychiatry at UCLA, and Paul Thompson, who is associate professor of neurology at the UCLA Laboratory of NeuroImaging, used a novel method of three-dimensional magnetic resonance imaging (MRI) to map the entire surface of the brain in people diagnosed with bipolar disorder. Everyone interested in the brain has been amazed by the quality of the images coming from the UCLA lab over the last six or seven years. (Graphics from the study, including the one above, are available online here.)
When the researchers compared the brains of bipolar patients on lithium with those of people without the disorder and those of bipolar patients not on lithium, they found that the volume of gray matter in the brains of those on lithium was as much as 15 percent higher in the cingulate and paralimbic regions of the brain, that are critical for attention, motivation and emotional control. There was no change in the amount of white matter, telling us that these effects are unlikely to be either artifacts or swelling of the brain.
These are extraordinary findings that may help explain how lithium works. If lithium increases the amount of gray matter in specific regions of the brain, this may suggest that existing gray matter in these regions may be underused or dysfunctional in people with bipolar disorder.
Conventional MRI studies in bipolar disorder measured the total volume of the brain, but these new imaging techniques employ high-resolution MRI and cortical pattern-matching methods to map gray matter differences that are so precise that they can pick up subtle differences in brain structure and this is the first time that researchers have been able to look at specific regions of the brain in people with bipolar disorder, and examine the effects of treatment.
The researchers at UCLA analyzed MRI scans of 28 adults with bipolar disorder, 20 of whom were lithium-treated, and 28 healthy control subjects collected by collaborators at the University of Pittsburgh. The analysis involved detailed spatial analyses of the distribution of gray matter by measuring local volumes of gray matter at thousands of locations in the brain.
This is superb research, and one of the signs of good research is that it raises yet more questions:
- We do not know whether these effects on gray matter persist once the medicine is stopped.
- Neither do we know whether the same effect might occur in other illnesses in which there is loss of gray matter. It may just be that lithium corrects an abnormality that is specific to bipolar disorder. That being said, there is recent evidence that lithium may be neuroprotective in a mouse model of Alzheimer’s disease.
- We also do not know if these brain changes correlate with clinical improvement.
- Lithium can have a lot of side effects, so we shall also need to factor that into the equation.
- We also need to know whether other medicines – or any other kind of therapy – might produce similar effects: there are already several medicines that have been shown to do something similar in some animals.
It’s still a bit too early to suggest putting lithium in the water supply…
A Major Breakthrough in Neurogenesis Research
I have written a lot about adult neurogenesis, because it is so incredibly important.
When most of us were in school were taught that the brain is a static structure. That you are born with a certain number of neurons, that constitutes your neural “stash.” And after the age of five you would lose a hundred thousand neurons a day, and if you drank too many martinis it would be two hundred thousand a day. “Facts” and figures repeated from one textbook to another for fifty years. And quite wrong.
Ten years ago it was discovered that there are neural stem cells in the hippocampi of adult rodents. A study published in 1998 provided some evidence that neurogenesis takes place in the adult human hippocampus, but the idea that neurogenesis takes place in adult humans has remained contentious.
Now, an advance online publication on the website of the journal Science provides evidence that neurogenesis may also occur in the olfactory bulb of the human brain.
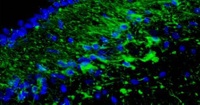
The whole article, including the pictures is available here. The picture at the top of this article shows new cells appearing in the olfactor bulb.
The investigators examined the rostral migratory stream (RMS) which is the main pathway by which newly born cells from the subventricular zone (SVZ) reach the olfactory bulb in rodents. The researchers discovered that there is a human RMS containing neuroblasts, a.k.a. neural stem cells.
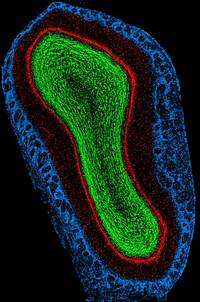
(This is a rat olfactory bulb)
Maurice Curtis and his colleagues examined the brains of cancer patients who had recently died, after having been previously injected with bromodeoxyuridine (BrdU), a chemical that is incorporated into newly synthesized DNA. Cell biologists and oncologists have used the method for years to visualize and monitor the growth of tumors. The researchers found BrdU-positive cells in the olfactory bulbs of the patients’ brains, indicating that they contained newly-generated neurons.
The team then used antibody staining to show that the neuroblasts begin to differentiate into olfactory neurons while migrating through the rostral migratory stream. Upon arriving at the bulb, the cells continued to differentiate, forming mature olfactory neurons.
The patients whose brains were examined were between 38-70 years of age, so the findings show that neurogenesis may occur throughout the duration of the human lifespan. The function of these newly generated cells is unclear, but they may be involved in recognizing and remembering new smells in the later years of life.
The researchers also have preliminary unpublished data that the stem cells not only migrate to the olfactory bulb, but also leave the RMS and migrate into the basal ganglia and cerebral cortex. This is significant, because parts of the basal ganglia degenerate in movement disorders such as Parkinson’s Disease, and specific regions of the cortex degenerate in Alzheimer’s. The possibility that stem cells enter these regions from the RMS could therefore provide a means for developing new treatments for neurodegenerative diseases.
So although at the moment new neurons are only known to be created in a small number of ancient structures in the brain, but that may well change, since the cells are marching over there from regions around the ventricles. After all, why would Nature, the Universe or God have left neural stem cells sitting there unless it was for a good reason? And if adult neurogenesis can be demonstrated in other parts of the brain, then what? An end to the stem cell debates? If the stem cells are already present in the brain, the effort can be directed toward activating and directing them. Could we continue generating new neurons to stave off the dementing illnesses, or is that just science fiction?
The answer is that science fiction is fast becoming science fact. This research will need to be replicated, but I know of several other labs that have already accumulated some similar data to this new paper in Science.
Leg Length and Cognitive Reserve
I recently mentioned the "Barker Hypothesis" which says that fetal malnutrition is associated with many physical problems later in life.
Well the difficulties may not only be physical.
I would like to tell you about an important concept that we call "Cognitive reserve." This can be thought of as our cognitive resilience. This first came to light almost twenty years ago when a post-mortem study of 137 elderly people was published in the Annals of Neurology, and confirmed something that we had suspected for years: there was a large discrepancy between the degree of Alzheimer’s disease neuropathology and the clinical manifestations of the disease. Some people had extensive pathology but they clinically had no or very little manifestations of the disease. The investigators also showed that these people had higher brain
weights and greater number of neurons compared with age-matched
controls. This lead to the idea that they had a greater "reserve." This is why building your brain throughout life is thought to reduce the ce of cognitive impaitrment later on.
Studies have shown that childhood cognition, educational attainment and adult occupation all independently contribute to cognitive reserve, and more recently it has been confirmed that education and the complexity of a person’s occupation may both slow the rate of decline in people who already have Alzheimer’s disease.
Although height is in part genetically determined, shorter leg length has been found to be associated with an adverse environment in early childhood. In a recent study of older Afro-Caribbean people living in London, shorter leg length was significantly associated with cognitive impairment, leading to the suggestion that shorter leg length may be a marker of early life stressors that then result in reduced cognitive reserve.
It is also worth recalling our discussion about the association between growth hormone and intelligence in children and between intelligence and head size.
And nutrition is one of the determinants of growth hormone synthesis and release.
Naturally this does not mean that less tall people will all get Alzheimer’s disease. But these observations have a number of practical consequences. They re-emphasize the importance of good nutrition during pregnancy: something that is simply not available to over a third of the world’s population. They also help us to identify some of the people who would most benefit from strategies to increase their cognitive reserve and to avoid some of the things that can strip it away from them.
Healthy Aging
I have talked about the small number of simple steps that can dramatically reduce your risk of getting congnitive decline as your get older and some new evidence to show the benefits of non-drug treatments for dementia. I am pleased to say that my conclusions have just been supported by an editorial in the Journal of the American Medical Association.
I would like to let you know about another great resource: the International Council on Active Aging (ICAA) which has produced a great package of action items that are all rooted in good quality scientific research. The list is very similar to the ones that I have created for you here, and are very precise.
- Invest in good shoes and socks
- Play games
- Walk
- Increases your physical activity
- Do exercises to improve your balance
- Get regular eye checks, not only for corrective lenses, but to be checked for early evidence of diabetes or high blood pressure
- Seek out friends family and neighbors
- Modify your diet toward a "Mediterranean" one
- Laugh
- Get enought sleep
Whatever your age, I urge you to spend a few minutes working on a simple plan that will fit your schedule: your mind and body, family and friends will thank you forever.
Learning to Tango

As a youngster I was introduced to most of the social graces: piano lessons – which sadly I hated – shooting, horse riding, fencing and ballroom dancing. And I just loved to tango!
Now I learn that it is, perhaps, something that more people should try.
Colleagues from the University of Turin used functional magnetic resonance imaging to study the hypothesis that simply focusing attention on walking could modify the activity of specific regions of the brain. But instead of using regular walking they taught people to tango. (The whole paper is available online as a free download.)
If you think about it for a moment, regular walking is an automatic process that you learned as a small child. It involves a series of structure in the deep – subcortical – regions of the brain and the spinal cord. The researchers got their experimental subjects to learn the dance by a combination of physical and mental practice. They were asked to perform the basic steps of the tango followed by imagining that – without moving – they were doing the steps.
The experiment showed that the training was associated with an expansion of regions of the brain involved in imagining movement. After the training the visual imagery gradually gave way to motor and kinesthetic ones.
This makes good sense: we normally begin by visualizing and then over time a motor skill like this becomes automatic. I’ve known good dancers who could flip from one dance to another without a moment’s thought.
This new finding suggests that rehabilitation of people who have lost the ability to walk should involve not just the motor act of walking, but also visualization.
But notice that the two processes – visualization and motor learning are separate. This is another nail in the coffin of the popular idea that your brain cannot tell the difference between a real and an imagined activity.
It also provides further evidence that both mental and physical activities can expand and activate regions of the brain.
And what a fun way to do it!
“The truest expression of a people is in its dance and in its music. Bodies never lie.”
–Agnes de Mille (American Choreographer, 1905-1993)
Brain Gain
We have previously discussed how a relatively small number of strategies can dramatically reduce your risk of cognitive decline as you get older.
Our recommendations are firmly buttressed by a most important article available for free download at the website of the Journal of the American Medical Association.
We already knew that cognitive training can improve cognitive abilities in older adults but nobody had established the effects of cognitive training on everyday function.
Sherry Willis of Pennsylvania State University led a team of scientists that followed a group of 2,832 adults, aged 65 and older -mean age 73.6 years – who were still living independently between 1998 and 2004. The seniors came from all walks of life, races, and parts of the country, including Birmingham, Alabama; Detroit, Michigan; Boston, Massachusetts and three other major cities. They all had one thing in common when the study commenced: they had no signs of cognitive impairment.
The researchers divided them into four groups of roughly 700 each: three groups that would receive training in either memory (verbal episodic memory), inductive reasoning or speed of processing (visual search and identification) with 4-session booster training at 11 and 35 months after training, and one that would serve as a control.
The memory training program consisted of mnemonic strategies for remembering word lists or texts, such as associating various words, visualizing them or organizing them in specific ways. Reasoning training taught the participants how to spot the pattern in a series, such as “a c e g i… .” The researchers boosted the subjects’ processing speed via practice, practice, practice in identifying an object on a screen after increasingly short exposures.
Over the course of the next five years the researchers asked participants to appraise their skills and to report whether the training had helped with everyday tasks. They also independently evaluated the subjects’ skills in things like finding items in a medicine cabinet. After training, 87 percent of the speed trainees, 74 percent of the reason trainees and 26 percent of memory trainees showed immediate improvement. That advantage over their untrained peers persisted over the next five years.
The training seemed to largely offset the cognitive decline suffered by nearly all of the controls as the years wore on. By the fifth year, significant skill gaps had opened between the people who had done the training and their untrained peers.
It is not enough to continue to do the crossword or sudoku puzzles. The brain must be continually stretched and challenged. It seems that to drive this effect, you have to practice things that you don’t like or things you don’t regularly practice.
Many of us have spent years working on new training strategies, and this research shows just how valuable cognitive training can be for all of us.







