Violence and Diet
We have talked before about the link between nutrition and violence.
The evidence has continued to mount and I was pleased to see that the Wellcome Trust is funding trials in three British prisons to investigate the link between nutrition and behavior. This is a placebo study that will examine which nutrients are most important and at what dosage.
Volunteers from three young offenders institutions housing male prisoners aged 16 to 21 will take nutritional supplements in addition to their normal choice of food to ensure they receive the necessary vitamins, minerals and essential fatty acids to meet daily guidelines. The investigators will monitor how levels of nutrients affect a range of behaviors including violence, drug-related offences and incidents of self-harm.
The new trials build on previous research published in the British Journal of Psychiatry that was conducted at the then maximum security Young Offenders Institution in Aylesbury, Buckinghamshire. That study was funded by Natural Justice, a research charity that investigates the social and physical causes of offending behavior. Nutritional supplements – 2 grams per day of the omega-3 fatty acids EPA and DHA for three months – were given to ensure that inmates’ diets reached recommended UK dietary standards. The researchers found that the prisoners who consumed the active nutrient capsule committed on average 26% fewer disciplinary offenses overall than those taking the placebo and 37% fewer violent offenses.
The most likely reason why supplements can have such a large effect is because the proper functioning of nerve cell membranes and signaling molecules depends upon adequate amounts of minerals, vitamins and essential fatty acids in the diet.
This is extremely important work. Clearly nutrition is not the only driver of violence but it has been wondered for a long time whether the industrialization of our diets has contributed to the enormous rise in violent crime between the 1950s and 1970s.
“Violence is the last resort of the incompetent.”
Isaac Asimov (Russian-born American Biochemist and Writer, 1920-1992)
“Blessings crown the head of the righteous, but violence overwhelms the mouth of the wicked.”
–The Bible (Proverbs 10:6)
“Peace cannot be achieved through violence, it can only be attained through understanding.”
–Ralph Waldo Emerson (American Poet and Essayist, 1803-1882)
Antioxidants May Raise Cancer Risk?

Regular readers will know that I have for some years now been raising a red flag the wholesale promotion of antioxidants.
The trouble is this: antioxidants are supposed to help rid us of some of the free radicals that have been implicated in a small number of diseases, and may also play a role in some of the physical aspects of aging. However, free radicals are also some of the major cancer killers in the body, so eradicating them – even if it were possible – hardly seems like a good idea.
According to an analysis of a dozen studies including more than 100,000 patients in the Mayo Clinic Proceedings taking antioxidant supplements do not reduce cancer risk.
In fact smokers who take beta carotene supplements could be increasing their risk of smoking-related cancer and death.
Different antioxidants have different effects, and their effects may also vary depending on the part of the body involved.
The researchers looked at 12 trials that compared antioxidant supplements with placebo on cancer incidence and mortality. Antioxidant supplements did not reduce the risk of cancer. When they looked separately at beta carotene, they found the nutrient actually increased cancer risk by 10 percent among smokers. There was also a trend toward a greater risk of dying from cancer with beta carotene supplementation.
Selenium supplements reduced cancer risk by 23 percent among men, the researchers found, but had no effect on women. While vitamin E had no anti-cancer effect overall, supplementation with the nutrient was tied to a 13 percent lower prostate cancer risk.
A large study looking at vitamin E supplementation for prostate cancer is currently underway. While future studies of beta carotene and vitamin E for cancer prevention are very unlikely to show effectiveness, it would be worth doing further studies on selenium.
The moral of the story: we should be going for a balanced diet and a balanced life in general rather than putting our hopes in an over-simplified nutritional message.
Grapefruits, Medicines and Medical Correspondents

Mark Twain once said:
“Be careful of reading health books, you might die of a misprint.”
I was thinking about that as I was watching a TV show earlier.
I have spoken before about the frustration of many of us about the quality and accuracy of some media medical correspondents. Though every show has a disclaimer about the importance of discussing any issue with a health care provider, it is really unfortunate to present inaccurate data that could needlessly alarm people.
I will immediately put my hand up and say that I have done more than my share of media work, not just in the United States and Great Britain, but also in countries from Finland to Australia and twenty or thirty more in between. And I may well have misspoken at some time or other. Even the most well intentioned people sometimes make slips, and it is especially easy when you are in a studio and you know that the clock is counting down.
But that stress makes it all the more important to have accurate material prepared in advance so that slip-ups don’t happen.
Today’s piece was about a story that pink grapefruit may not interact with some medications. The correspondent rightly said that any type of grapefruit may interact with some medications, but then said that there was an interaction in the stomach. This is not correct and could be very confusing.
The issue is that grapefruit juice may induce the enzyme complex cytochrome P450 3A4 in the liver and intestine. So if you or a medication that is metabolized by the enzyme, grapefruit juice may lower the plasma level of the drug, making it less effective. This is another example of the importance of telling your health care provider about ANYTHING that you eat or drink, in addition to listing any herbs and supplements that you take.
Here is a list of some of the more common medicines metabolized by cytochrome P450 CYP3A4:
Alprazolam
Amiodarone
Amlodipine
Aripiprazole
Astemizole
Atorvastatin
Buspirone
Cafergot
Chlorpheniramine
Cimetidine
Cisapride
Clarithromycin
Cocaine
Codeine
Cyclosporine
Dapsone
Dexamethasone
Dextromethorphan
Diazepam
Diltiazem
Domperidone
Erythromycin
Estradiol
Felodipine
Fentanyl
Finasteride
Fluconazole
Fluvoxamine
Grapefruit juice
Faloperidol
Hydrocortisone
Iindinavir
Itraconazole
Ketoconazole
Lidocaine
Lovastatin
Methadone
Midazolam
Mifepristone
Nefazodone
Nifedipine
Nitrendipine
Norfluoxetine
Ondansetron
Pimozide
Progesterone
Propranolol
Quetiapine
Quinidine
Quinine
Risperidone
Ritonavir
Sildenafil
Simvastatin
Tacrolimus
Tamoxifen
Taxol
Telithromycin
Terfenadine
Testosterone
Trazodone
Triazolam
Verapamil
Vincristine
Ziprasidone
Zolpidem
Broccoli and Skin Cancer

This one is going to launch a thousand gags on the late night talk shows, but it is actually quite serious.
Despite what you hear on some of those infomercials, there is a strong link between ultraviolet radiation (UVR) and many kinds of skin cancer. You can even use ultraviolet radiation to induce cancerous change in cells cultures in a Petri dish.
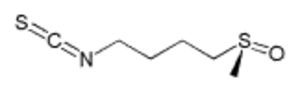
In an article from Johns Hopkins University published in the Proceedings of the National Academy of Sciences damaging effects of UVR can be significantly reduced by the topical application of a broccoli extract called sulforaphane that comes from broccoli sprouts. Sulforaphane was first identified over 15 years ago, and it has been shown to play a role in preventing the development of several types of tumors that can be induced by cancer-causing chemicals. It may also have a role
in fighting some established tumors.
The research involved both animal and human studies, and showed that the level of erythema (skin reddening) caused by UVR is substantially reduced when this extract is applied to the skin.
The broccoli extract is not acting like a sunscreen; it does not absorb the UVR, neither does it stop it from entering the skin. Instead it enters the cells and switches on the production of several enzymes that protect cells from UV damage. The result is that the protective effect is sustained for days after the extract has been removed.
The advantage of this is that it is much longer-lasting than any sunscreen – several days, in fact. The scientists said the protection is still there when no extract is present on/in the skin.
The researchers first tested sulforaphane on mouse models of skin cancer, and then on six healthy human volunteers.
Each of the volunteers had small patch of skin exposed to a pulse of UVR. Some of the patches were treated with the broccoli extract while others were not.
At the highest UVR dosages, UVR-induced redness and inflammation was on average 37% lower when the extract had been applied, and the protection was sustained for at least three days. They also found that protection varied greatly depending on the person – protection ranged from 8% to 78%.
These variation may be due to the volunteers’ different skin types, dietary habits and genetic differences.
In these trials, the conventional sunscreens did not provide significant protection.
This research is important for several reasons:
- The research re-emphasizes the importance of recognizing inter-individual differences. An approach that works for one person may not help another
- There are many times in life when we cannot do much to prevent something bad happening to us: radiation, stress or somebody being mean. The new approach s not just to prevent exposure, but also to work on resilience: how can we stop ourselves from having a bad reaction? The whole of us, from our cells to our soul?
- It is inevitable that people will start telling you that broccoli is the way to protect yourself against skin cancer, and I am just waiting for the advertisements to start coming in. Do not be fooled! This research involves a specific extract applied to a precise area of skin. As far as we know, it does not apply to eating broccoli
Herbal Remedies

Edzard Ernst’s group at Peninsula Medical School, Universities of Exeter in England has published another study that is critical of one aspect of complementary medicine.
They set out to summarize and evaluate the evidence from randomized clinical trials for the effectiveness of individualized herbal medicine.
They conducted a search of electronic databases and also contacted experts in the field to identify randomized controlled clinical trials of individualized herbal medicine. They then conducted an independent data extraction and assessed the quality of the studies.
They found three randomized clinical trials of individualized herbal medicine. They concluded that statistically non-significant trends favoring herbal remedies over placebo treatment in osteoarthritis of the knee probably resulted from large baseline differences and “regression to the mean.”
They also concluded that individualized treatment was superior to placebo in four of five outcome measures in the treatment of irritable bowel syndrome, but was inferior to standardized herbal treatment in all outcomes.
Finally individualized herbal treatment was no better than placebo in the prevention of chemotherapy-induced toxicity.
The final conclusion was that there is very little evidence regarding the effectiveness of individualized herbal medicine.
Though this result is rather gloomy, it is important not to throw out the baby with the bathwater.
The researchers did the right thing: they asked the experts and examined the published data. Yet every practitioner has seen herbal remedies that seem to help certain specific conditions. So my take on this study is not to abandon herbalism, but to realize that there is a great deal more research to be done.
Non-pharmacological and Lifestyle Approaches to Attention-Deficit/Hyperactivity Disorder: 3. Herbal Remedies
Herbal medicines are crude drugs of vegetable or plant origin, which are used for the prevention or the treatment of disease states or to attain or maintain a condition of improved health. The use of herbs can be divided into four main categories:
- Folk Herbalism: You may well have come into contact with this: we use the term folk herbalism to describe traditional healing methods based upon plants. Many of our ancestors brought folk remedies from Europe or learned of healing herbs from Native Americans
- Western Medical Herbalism: This has been developing in Europe over the last century, and represents an attempt to classify and codify medically useful herbs
- Ayurvedic Herbalism: This is the ancient traditional herbalism of the Indian Subcontinent. Some Ayurvedic herbs have found their way into conventional medicine. The best-known example is the drug reserpine, which was at one time used for treating high blood pressure and mania. It was extracted from the Himalayan bush Rauwolfia serpentina. Ayurvedic herbs are most readily available in cities with large Indian populations
- Chinese Herbalism: One of the five branches of traditional Chinese medicine, there are many thousands of Chinese herbs, which are usually administered in complex combinations. Though most are prepared with close attention to detail, there have been many reports in the literature of adulteration of Chinese herbs with heavy metals.
Herbs are used directly as teas or extracts, or they may be used in the production of drugs. Around 25% of the prescription drugs sold in the United States are plant based. Two good examples are aspirin, which was originally extracted from the bark of the willow tree and digoxin, a purified form of digitalis, from the foxglove. Many more herbal ingredients are present in over-the-counter medicines, particularly in laxatives.
Herbal medicines are considered to be dietary supplements; therefore they are not required to meet the standard for drugs specified in Federal Food, Drug, and Cosmetic Acts. They are only required to meet the standards set forth in the 1994 Dietary Supplement and Health Education Act (DSHEA). Furthermore, they may be produced without complying with standards for good manufacturing practice. They also do not need the prior approval of safety and efficacy by the Food and Drug Administration (FDA). So long as the term “disease” is not on the label, the FDA has no regulatory powers.
Many herbal products have been used to treat Attention-Deficit/Hyperactivity Disorder (ADHD), and there are hundreds of websites claiming that their products are effective. However the research is often not quite what it seems. Some sites simply use loads of testimonials, but happily there are others who have products supported by empirical research. The use of herbal remedies in ADHD is popular in Europe, although the problem is less widely recognized in that part of the world. The most popular include sedative herbs, herbs used to enhance brain function, antioxidants and stimulants. The last category is herbs that are used to treat other symptoms, particularly mood disorders that are very common in adults with ADHD.
Medical reviews of herbal remedies do not always make the point that herbalists typically individualize the treatment for the individual. So two people with apparently similar symptoms may receive different treatments.
They are often used together with a whole-foods diet, high in protein and complex carbohydrates and low in simple sugars.
Sedative herbs
Sedative or calming herbs are amongst the most popular herbal options for treating ADHD. These include:
Chamomile
Hops
Lemon balm
Valerian
Kava kava
Sedative herbs may be helpful in promoting sleep in children who have trouble falling asleep. They are generally safe, but there is little scientific evidence that they can improve daytime behavior in children with ADHD, and it is important to be aware that they are medicines that do have side effects and may interact with each other and with prescription medicines. Here is a chart of some interactions between medicinal herbs and drugs.
Brain “enhancing” herbs
A small open study of 36 children with ADHD who were treated with a combination herbal combination of Panax quinquefolium (200 mg) + Ginkgo biloba (50 mg) twice daily for 4 weeks, reported an improvement in 74% at the end of the study. The combination was marketed as AD-FX, but it has recently become difficult to obtain it in the United States for commercial rather than legal reason. Gingko has become one of the most popular herbs given to children with ADHD, but more research is necessary: there is enormous variability in the quality of commercially available herbs. Gingko may also cause bleeding in people at risk of it. It was interesting that Panax was included: there are reorts of people becoming more hyperactive in overdose.
Antioxidant herbs
Pycnogenol (pine bark extract) has been tested in a randomized, controlled trial involving 61 children who received either 1 mg/kg/day Pycnogenol or placebo for 4 weeks. In this study, Pycnogenol was associated with a significant reduction of hyperactivity, improved attention, eye-hand coordination, and concentration. When the herb was stopped, the symptoms returned within a month. An earlier short study in adults had failed to find an effect, but it could have been because of the dose used.
Stimulant herbs
Coffee, tea, and cocoa all have stimulant effects that tend to be milder than medications. Caffeine helped spatial learning deficits in an animal model of ADHD, and there have been several small studies of caffeine, but most have failed to find much benefit. In a double-blind cross-over trial of just 8 boys with ADHD modest doses of caffeine (160 mg, roughly equivalent to 1.5 cups of coffee) were less effective than large doses of methylphenidate (20 mg) in improving behavior. Although many adults self-medicate with coffee, few use it in children with ADHD. And it can, of course, cause insomnia and anxiety.
Chinese herbalists use multiple combinations and there have been some publications (1, 2, 3,) suggesting that further work on Chinese herbal medicines might be worthwhile. The methods of some Chinese medical research studies are rather different from those done in the West, so we need to be a little cautious.
There are some herbs and supplements that are linked to an increase in symptoms of hyperactivity including:
Yohimbine
Korean ginseng
Siberian ginseng
American ginseng
L-glutamine
Conclusions
Although there is some data, and a lot of practical experience, it is still not clear who is likely to benefit from which herbal remedy. The variable quality of herbal products and the risk that some may be contaminated has added to the uncertainty. It is also important to remember that herbs are drugs, and that they can interact with each other and with prescription medicines, and that just because they are natural, does not necessarily mean that they are safe.
After all, deadly nightshade, arsenic and hurricanes are natural as well.
Non-pharmacological and Lifestyle Approaches to Attention-Deficit/Hyperactivity Disorder: 2. Nutritional Supplements

It sometimes surprises people to learn that the FDA does not currently regulate the production of supplements and herbal products. Therefore their purity and contents may vary considerably. Though most of them are fine, there have been endless examples of supplements that contained no active ingredients or were adulterated with heavy metals or prescription medicines.
Amino Acid Supplementation
The idea of using amino acid supplementation is based on reports of low levels of amino acids in ADHD, including the particular amino acids – tyrosine, phenylalanine and tryptophan – that are the building blocks of catecholamines and serotonin.
Several open and controlled studies in both adults and children have reported a short-term benefit from tryptophan (precursor of serotonin), tyrosine (precursor of catecholamines), or phenylalanine (precursor of catecholamines) and S-adenosyl-methionine supplementation.
However, no lasting benefit beyond 2–3 months has been demonstrated: both children and adults develop tolerance. Even short term, there is a lot of dispute about whether these supplements work at all.
Vitamins
Three strategies for vitamin supplementation are:
- Recommended Daily Allowance (RDA) multivitamin preparations
- Megavitamin multiple combinations
- Megadoses of specific vitamins
The first is not controversial, although there is always a discussion about whether the RDA’s is correct. There has not been any credible research on the effects of his kind of supplementation in diagnosed ADHD even though some reports suggest mild deficiencies in diet and blood levels. There is some evidence that micro-nutrient supplementation will help the intelligence and ability to concentrate in children without ADHD, but whether the same holds in ADHD, we simply do not know.
The second strategy, megavitamin multiple combinations, has not been found effective in double-blind placebo-controlled short (2 weeks) and longer (up to 6 months) trials in ADHD and the related comorbidity of learning disorder, although it is always possible that the researchers did not use the correct mixture of vitamins and minerals.
As things stand megavitamin combinations do not seem worth pursuing for children or adults, and some may be risky.
The third strategy, the use of single vitamins in huge doses to alter neural metabolism has not been explored despite some encouraging early reports.
Minerals
Deficiencies of iron, zinc, and magnesium have been noted more commonly among children with ADHD than among normal children.
Iron
Iron is a coenzyme involved in the synthesis of catecholamines, so there has been a lot of interest in iron deficiency as a possible cause of a number of neurocognitive problems. Iron deficiency may be due to poor diet, celiac disease, excessive milk ingestion, infection, gastrointestinal losses or lead. And of course in adults, many women are chronically iron deficient. Children with ADHD may have lower iron stores and in a study of nearly 100 children, there was a significant inverse correlation between ferritin levels and scores on a standard ADHD rating scale.
Zinc
Zinc is a co-factor for 100 enzymes, many involved in neural metabolism. It is also necessary for fatty acid absorption and for the production of melatonin, the light–related hormone that helps regulate dopamine function. Zinc is so important for the normal functioning of the brain that it is plausible that deficiency would adversely affect behavior and that restoring optimal levels may provide some benefit.
Zinc has been found to be lower in some children with ADHD. In a study of 44 children with diagnosed ADHD, zinc had a significant inverse correlation with attention, even controlling for gender, age, income, and diagnostic subtype. In large randomized, controlled trial, children given zinc sulfate (150 mg/day) or placebo, the zinc-takers had significantly more improvement for impulsive behavior and socialization; the best response was observed in those children who had low zinc levels to begin with. We do not know if using mega-doses of zinc will confer any benefit.
Magnesium
Magnesium deficiency can cause a wide spectrum of neurological and psychiatric disturbances and can result from a many factors including increased requirement during childhood.
In one study, 30 out of 52 children with ADHD had low levels of magnesium in their red blood cells. An open-label study supplementing them with 100 mg daily of magnesium and viamin B6 for 3-24 weeks led to reduced symptoms of hyper-excitability (physical aggression, instability, attention to school work, muscle tension and spasms) after 1 to 6 months of treatment.
Conclusions
It is usually just enough to ensure that children with ADHD have a decent diet. But in some it may be necessary to take supplements to ensure that they are getting an adequate dietary intake of iron, zinc, and magnesium.
Other Supplements
Essential Fatty Acid Supplementation
The membranes of nerve cells are composed of phospholipids containing large amounts of polyunsaturated fatty acids, especially the n-3 and n-6 (or omega-3 and omega-6) acids. What these terms mean is simply that the first unsaturated bond is 3 or 6 carbons, respectively, from the noncarboxyl “tail” of the molecule). Humans cannot manufacture these fatty acids and hence are “essential” and needed in the diet. Essential fatty acids (EFAs) are also metabolized to prostaglandins and other eicosanoids, which modify many metabolic processes, activate eicosanoid receptors, and interact with pro-inflammatory cytokines.
Rats that have low levels of omega-3 fatty acids in their brains, tend to be hyperkinetic.
Fish oil/omega-3 fatty acids
Children with lower levels of omega-3 fatty acids seem to have significantly more behavioral problems, temper tantrums, and learning, health, and sleep problems than did those with high proportions of omega-3 fatty acids.
In a 4-month trial of 63 children with ADHD, DHA (one of the essential fatty acids found in fish oil) supplements alone had no significant impact on behavior. In a randomized, controlled trial of fatty acids supplementation for 117 children with developmental coordination disorder, there were significant improvements for children on active treatment in reading, spelling, and behavior over 3 months of treatment. But when the tratments were crossed over, similar changes were seen in the placebo group. We definitely need more research on fish oils. Most experts think that children need around 1000mg/day and adults up to 3000mg/day.
There may be a downside: large doses of fish oil may inhibit platelet aggregation and increase the risk of bleeding; its use should be discontinued 48 hours before having surgery. Many people do not like the taste of fish oil, though in capsules that is not normally a problem.
Gamma-Linolenic Acid
Evening primrose oil contains gamma linoleic acid. Two small randomized, controlled trials conducted in the 1980s showed only marginal benefits of evening primrose oil for children with ADHD.
L-Carnitine
The mixed results with essential fatty acids might have something to do with the transport and metabolism of the fatty acids. One essential component of these metabolic pathways is L-carnitine, so it too has been tried in ADHD, but so far there are no good trials to help us.
Glyconutritional Supplements
Glyconutritional supplement contains basic saccharides necessary for cell communication and the formation of glycoproteins and glycolipids.
In an open trial of glyconutritional and phytonutritional (flash freeze-dried fruits and vegetables) supplementation with 17 ADHD children, researchers found significant reductions in parent ratings of inattention, hyperactivity, impulsivity, and oppositional symptoms, with similar trends on teacher ratings. In a second open trial of the same supplements in 18 children, researchers found reductions in parent inattention ratings from 2.47 to 2.05 and hyperactivity-impulsivity ratings from 2.23 to 1.54. There was an impressive statistical value for this trial and the results were sustained for 6 weeks. However, a third open trial reportedly failed to duplicate such results. There have not been any reported trials of glyconutritional supplements in adults.
Dimethylaminoethanol
Dimethylaminoethanol (DMAE) has several accepted names, including deanol and dimethylethanolamine. It is the immediate precursor of choline (trimethylaminoethanol) and is claimed to increase production of acetylcholine. There have been several studies claiming a small effect on vigilance, alertness and mood, but there are questions about its safety.
Melatonin
Melatonin helps regulate dopamine function in the brain, so it has been a natural candidate for the treatment of ADHD. A randomized, controlled trial 25 children with ADHD and chronic insomnia were either given melatonin (5 mg) or placebo daily at 6pm; the melatonin significantly improved sleep onset, decreased sleep latency, and increased total sleep time. Although there was no significant change in ADHD behavior over the 4-week study, all the parents in the trial felt the improvements in sleep were enough to justify continuing to give it for 1 year after the study. These results have been replicated in another study: melatonin helps with sleep problems in chdlren wth ADHD, but had no efect on problem behavior, cognitive performance or quaity of life. Melatonin may be helpful for children with ADHD who have trouble with sleep.
As you can see there are a great many options, but despite all those articles in magazines and online that promise the earth, the evidence for most of the approaches is thin.
At the moment the best option that may help seems to be fish oils. Choosing the best supplement is not easy, but the one for which there is most evidence, and which seems to be the most pure and mercury-free is OmegaBrite.
Risky Advice About Bipolar Disorder
Sad to say, I see a lot of articles on medical topics that don’t make much sense. Most are well-meaning so I usually just let them go unless the suggestions are dangerous or unwise. I have just seen an unfortunate example of both.
The writer is talking about natural treatments for depression and bipolar disorder. He or she first divides depression into three groups: mild, major and severe.
I have not seen that done in many years and it betrays a real misunderstanding of the illness. People with genuine depression or bipolar disorder can get very ill very quickly, and these are illnesses in which as many as a quarter to a half of all sufferers attempt suicide. So it is risky to minimize the severity of the illness.
The writer then talks about “Bipolar Depression is a severe condition of depression that has manic undertones.”
This is simply not accurate. The “manic phase” of bipolar II disorder may be very mild, or present as intermittent anxiety or irritability. There is a great deal of discussion going on about the clinical features of all the different forms of bipolar disorder as we begin work on DSM-V. He or she appears here to be talking about “Mixed states,” about which, as it happens, I shall be lecturing tomorrow.
The author deserves kudos for saying that medications may be necessary, but the potentially dangerous thing was the advice to use St. John’s Wort in “Mild” cases of bipolar disorder. St. John’s Wort may have a role in the treatment of mild to moderate depression: the experts are still deliberating about that. But the problem of using it in bipolar disorder is that it may precipitate mania. One of several reasons for the changing clinical features of bipolar disorder in recent years is the over-prescription of antidepressants and self-medication. It is always difficult to prove causality, but here are a few papers on the dangers of using St. John’s Wort in people who may have bipolar disorder: 1, 2, 3, 4, 5, 6.
Integrated Medicine constantly uses conventional medicine together with natural approaches, and respects the psychological, subtle and spiritual aspects of any life challenge. But have to be very careful about how we combine different approaches so that we don’t do more harm than good.
Be careful of advice that you read online!
Tea and Milk

Growing up in England, tea is a great deal more than a drink.
Always drunk hot, of course. No normal person would want it served cold.
It is a major social lubricant and is considered by most to be a separate food group. And the health benefits conferred by a nice cup of tea are now known to just about everyone in Britain.
But from an early age I knew that one day I would have to leave the country.
Why?
Because I could never abide the way in which the vast majority of tea drunk in England is destroyed by the addition of milk and sugar. There are even long technical debates about whether to add the milk before pouring in the tea or after? How fast to add the white stuff? How to stir it in?
Since I was knee high to a puppy I was always the odd one out, wanting nothing to do with this wanton destruction of a sublime beverage.
Which should always be enjoyed au naturel. The only thing that might ever sully a cup of fine Earl Grey or Darjeeling might be a little lemon. Anything else?
Yuk.
Well, it now transpires that this isn’t just a matter of taste buds.
A study just published in the European Heart Journal says it all in the title, “Addition of milk prevents vascular protective effects of tea.”
Tests on sixteen healthy postmenopausal female volunteers showed that black tea significantly improved the ability of the arteries to relax and expand, but adding milk completely blunts the effect. The research was supplemented by tests on rat blood vessels. Tea caused the muscle in the vessel wall to relax by producing nitric oxide from the endothelial cells that line blood vessels. Adding milk blocked the production of nitric oxide and the relaxation of the muscles.
Now bear in mind that they were testing black tea. The researchers are now looking at the potentially more potent green tea to see whether its effects are also blocked by milk.
The villain of the piece is a group of proteins called caseins, which they found interacted with the tea to decrease the concentration of catechins in the beverage. Catechins are the flavonoids in tea that mainly contribute to its protection against cardiovascular disease.
The moral of the story? Tea can be wonderful on so many levels. Not only does it taste good, but also it can do wonders for your health.
But please, please, please don’t lose all the benefits by sloshing in a load of milk!
Raw, naked tea is the way to go…
“Thank God for tea! What would the world do without tea? How did it exist? I am glad I was not born before tea.”
–Sydney Smith (English Clergyman and Essayist, 1771-1845)
Common Misconceptions About "Weight Loss" Supplements
My recent comments about chromium, the penalties handed down over false weight loss claims and my inability to find any support for an apparent claim concerning probiotics and weight gain, have lead to a flurry of questions and helpful responses.
By far the most common has been surprise. Most people assumed that:
- These dietary supplements are regulated and that:
- They are therefore safe and
- They have had to demonstrate that they are effective
In fact all of those three assumptions are wrong.
I have just found a most helpful article that you can download for free.
Last October at the 2006 Annual Scientific Meeting of NAASO – the Obesity Society – the results of a collaborative research program by the University of Connecticut’s Center for Survey Research & Analysis (CSRA) in Stamford, Connecticut and the University of Pennsylvania’s Center for Weight Loss and Eating Disorders in Philadelphia were presented. GlaxoSmithKline (GSK) Consumer Healthcare funded the study.
Findings from this first national survey on the safety and regulation of dietary supplements for weight loss include:
- 65% believing that weight-loss products are tested for safety
- 63% believing that weight-loss products are tested for effectiveness
- 54% believing that weight-loss products are approved by the FDA
- 64% believing that manufacturers are required to include warnings about side effects
- 50% of African Americans and 49% of Hispanics were more likely than Whites of European origin (36%) to believe supplements are safer than OTC or prescription weight-loss drugs
Congressman John Dingell from Michigan has indicated that the new Congress will be re-visiting the issue of the FDA’s regulation of some of these supplements.
That would probably be wise.
Though as a very firm advocate for health freedom, I always worry when new regulations are proposed, simply because they sometimes lead to the baby being ejected with the bath water.
I shall continue to watch this developing story and to let you know how things develop.







