The Causes and Consequences of Insulin Resistance
I have spent so much time talking about insulin resistance becuase it is one of the greatest medical threats facing the world.
It is estimated that approximately 33% of the adult population of the United States is insulin resistant, and if left untreated many will develop diabetes, hypertension and an array of other problems. It is an epidemic that is expected to swamp most health care systems around the world, yet sadly it may in most cases be preventable.
There is an enormous literature on insulin resistance. As of this afternoon there are almost 33,000 scientific papers on the subject.
I created this graphic to try and summarize the key points about insulin resistance: the main factors that may cause it, as well as the most important medical consequences.

(Click on the graphic to expand it.)
The Main Causes of Insulin Resistance are:
- Aging
- Intra-abdominal obesity
- Inactivity
- Glucose intolerance
- Genetics
- Fetal malnutrition
- Cigarette smoking
- Some medications
The Main Consequences of Insulin Resistance are:
- Type 2 diabetes mellitus
- Hypertension
- Arteriosclerosis
- Polycystic ovarian syndrome
- Non alcoholic fatty liver disease
- Disturbances in the function of the vascular endothelium
- Elevations of triglycerides and cholesterol
- Disturbances of clotting
- Disturnaces in kidney function
- DIsturbances in one type of heart rhythm
- Elevated uric acide levels
- Some malignancies
This is probably not a complete list, but it gives you a very good idea of the reasons for looking for insulin resistance. Many – but not all – experts now recommend measuring insulin resistance in people at high risk of developing any of these medical problems.
We have good evidence that lifestyle changes can prevent the development of many of these dire consequences, so it is certainly something worth discussing with your health care provider.
Dying of a Broken Heart
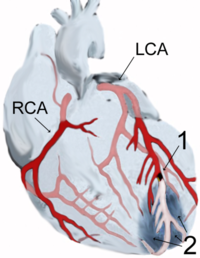
Some colleagues in London have discovered how intense stress may cause severe irregularities (arrhythmias) of the heart that could be fatal.
It has been known for some time that emotional trauma and psychological stress can precipitate cardiac arrhythmia and sudden death through over-activity of the sympathetic nervous system, the system usually associated with “Fight or flight.” It has also been known that people with preexisting heart disease are particularly at risk. This is one stereotype that is true: if someone with heart disease gets a bad shock, they may indeed die. It has been known for centuries that suffering a sudden unexpected bereavement can be a fatal stressor.
It is extremely important to understand how stress can affect the heart, and researchers at the Wellcome Trust Centre for Neuroimaging at University College London and the Brighton and Sussex Medical School have made an important breakthrough that has just been published in the Proceedings of the National Academy of Sciences. Measuring the electrical activity of the brain and heart at the same time, they discovered at the regions of the brain responsible for learning, memory and emotion can destabilise the cardiac muscle of someone who already has heart disease. These areas of the brain can participate in a “vicious cycle” with the heart.
The patients performed the task of counting backwards in sevens, which is for most people mildly stressful.
The researchers discovered that activity in “higher level” regions of the brain such as the cerebral cortex, not only reflected the responses of the heart to stress, but also became involved in a “feedback loop”, often worsening the situation by making the heart muscle less stable.
The regions of the brain responsible for regulating heart function can be unbalanced by stress, and it can be fatal.
It is further evidence that there is a constant “conversation” between the heart and the brain.
It is also the best evidence to date that comprehensive care of people with heart disease must include stress management.
And why wait until it’s too late?
Now is the time to start building your resilience to stress!
Fats, Inflammation and Depression

We have talked before about the associations between inflammation and psychiatric illnesses.
There is yet more evidence in the shape of a study just published in the journal Psychosomatic Medicine. by Janice K. Kiecolt-Glaser and her colleagues from Ohio State University College of Medicine in Columbus.
The study involved 43 older adults with a mean age of 66.67 years, and the results suggests that the imbalance of omega-6 and omega-3 fatty acids in the typical American diet could be associated with the sharp increase in heart disease and depression seen over the past century. The more omega-6 fatty acids people had in their blood compared with omega-3 fatty acid levels, the higher their levels of the inflammatory mediators tumor necrosis factor-alpha and interleukin-6, and the greater the chance that they would suffer from depression. These are the same inflammatory mediators associated with insulin resistance, type 2 diabetes and coronary artery disease, all of which are more common in depression. And depression is more common in diabetes, arthritis and coronary artery disease than expected.
Our hunter-gatherer ancestors consumed two or three times as much omega-6 as omega-3, but today the average Western diet contains 15- to 17-times more omega-6 than omega-3. There were 6 individuals in the study who had been diagnosed with major depression, and they had nearly 18 times as much omega-6 as omega-3 in their blood, compared with about 13 times as much for subjects who didn’t meet the criteria for major depression.
Depressed patients also had higher levels of tumor necrosis factor alpha, interleukin-6, and other inflammatory compounds. And as levels of depressive symptoms rose, so did the omega 6 and omega 3 ratio. So it seems as if the effects of diet and depression enhance each other. People who had few depressive symptoms and/or were on a well-balanced diet had low levels of inflammation in their blood. But when they became more depressed and their diets became worse – which is very common when people are depressed – then the inflammatory mediators in the blood surged.
Omega-3 fatty acids are found in foods such as fish, flax seed oil and walnuts, while omega-6 fatty acids are found in refined vegetable oils used to make everything from margarine to baked goods and snack foods. The amount of omega-6 fatty acids in the Western diet increased sharply once refined vegetable oils became part of the average diet in the early 20th century.
Depression alone is known to increase inflammation, the researchers note in their report, while a number of studies have found omega-3 supplements prevent depression.
So this more evidence for the value of eating fatty fish like salmon, mackerel or sardines two or three times a week, but be sure to avoid fish that may contain a lot of mercury. If you add more fruits and vegetables to your diet, you will also reduce your levels of omega-6 fatty acids.
I have just finished analyzing all the new literature on using fish oils for the prevention and treatment of psychological and psychiatric problems, and I am going to post my findings in the next couple of days.
Hot Flashes and High Blood Pressure

Many women experiencing hot flashes do feel as if their blood pressure is going up.
Well, there is some new research linking hot flashes and hypertension.
A hot flash (sometimes also referred to as a “hot flush” or, incorrectly a “night sweat”) is a symptom of changing hormone levels considered characteristic of menopause.
Hot flashes are typically experienced as a feeling of intense heat with sweating and rapid heartbeat,
and typically last from two to thirty minutes on each occasion. The event may be repeated a few times each week or up to a
dozen times a day, with the frequency reducing over time. Excessive
flushing can lead to the skin problem rosacea.
The study from Weill Cornell Medical College was published in the March/April issue of Menopause: The Journal of the North American Menopause Society.
The researchers used portable monitors to record the blood pressure of 154 New York City women, aged 18 to 65 (mean age of 46). The women had no previous cardiovascular disease and either mild hypertension or normal blood pressure. Fifty-one women reported experiencing hot flashes. These women were found to have an age-adjusted mean systolic awake blood pressure of 141 and a mean systolic sleep blood pressure of 129 — compared to 132 and 119, respectively, for women not reporting hot flashes. The results were highly significant. For people whose lives are not complete without a little “p,” the values were: p=0.004 and 0.007. The group differences for systolic blood pressure remained statistically significant after controlling for conventional hypertension risk factors, race/ethnicity, age and body mass index (BMI).
This is important research: High blood pressure is a major risk factor for heart disease, with the latter being responsible for half of all deaths among American women 50 and older.
We need to understand more about the mechanism linking blood pressure and hot flashes, but this research already suggests that women with flashes are at especially high risk. So if you know someone who ishaving them, make sure that they are having their blood pressure monitored on a regular basis.
Oral Health and Pointless Tests
I really like the Fox News Channel, but I sometimes worry about some of the medical advice that they dish out. The other morning I heard a dentist recommend that people should ask for a blood test to measure inflammation. She was saying that everyone should have the test, called C-Reactive Protein (CRP). This is really bad advice that is based on a fundamental misunderstanding of research data.
Yes, there is a link between dental disease and arteriosclerosis. And yes, there is a link between CRP and arteriosclerosis. But there is no good evidence that we should be measuring it on a routing basis.

The CRP Molecule
So what’s the problem about measuring CRP? If it is elevated, then what? There is no point in measuring anything at all unless you can take some action, or it guides prognosis. No good doctor would ever recommend treating a lab value. So if the CRP is elevated that would not just mean that it’s time to have a look at his or her pearly whites, it would mean a total body workup. There are dozens of causes for an elevated CRP. I know a lot about the topic: sixteen years ago I wrote one of the early scientific papers on CRP. It may go up if you have a fat tummy, have arthritis, allergies or if you are depressed, have fibromyalgia or irritable bowel syndrome. It also goes up as you get older, if you are physically inactive, or if you happen to have one of the genetic variants that can push it up.
In fact the questions of whether or not measuring CRP would improve coronary risk prediction is the subject of three papers and two editorials in the July 10, 2006 issue of the Archives of Internal Medicine and the July 4, 2006 issue of the Annals of Internal Medicine. In the July 10, 2006 issue of the Archives of Internal Medicine, a team led by Dr Aaron R. Folsom from the University of Minnesota in Minneapolis reported the results of the Atherosclerosis Risk in Communities (ARIC) study, which assessed the association of 19 novel risk markers with incident CHD in 15 792 adults followed up since 1987-1989.
The participants underwent a physical examination, including assessment of major risk factors, at the beginning of the study and every three years afterward. At four times during the follow-up period, researchers collected blood and DNA samples for analysis. Patients continue to be tracked for the development of CHD. Novel markers included measures of inflammation, endothelial function, fibrin formation, fibrinolysis, B vitamins, and antibodies to infectious agents.
Folsom concluded that:
“C-reactive protein level does not emerge as a clinically useful addition to basic risk-factor assessment for identifying patients at risk of a first CHD event. Routine screening is not warranted for any of the other 18 novel risk factors tested, either.”
Another study from Brigham and Women’s Hospital in Boston did suggest that CRP might be helpful in predicting coronary disease in some women. But in an editorial, George Davey Smith from the University of Bristol in England had this to say:
“There are many reasons for skepticism about the role of CRP as a predictor of CHD: CRP may not be causally related to CHD; it remains more expensive than asking patients about their health, lifestyle, and socioeconomic background; and it adds only modest additional predictive ability over conventional risk factors, even in Cook and colleagues’ (i.e. the Brigham and Women’s) study.”
The moral of the story? Random measurements of CRP have not been shown to be of much value.
And be a bit cautious about medical advice on Fox News.
Heart Attacks, Meaning and Relationships
I am a doctor who has spent my career trying to empower people to take control of their lives, to fulfill and exceed their potential and to achieve and maintain vibrant good health. So I have worked my backside off to help people to deal with disease. But the curing of maladies is only half of our task. We also need to learn why things go wrong and what they are trying to teach us. So many of us have become wedded to the idea that illnesses are nuisances to be conquered rather than inevitable parts of life that can help us to grow and develop.
If our search just keeps turning up negatives, “I keep getting sick because I have bad luck/was born under a bad sign/have bad karma,” then you may need a little help from a therapist to help with those negative cognitions.
Here is a remarkably interesting study published in the current issue of the Journal of Advanced Nursing, that buttresses years of my own clinical observations: A third of people who suffer myocardial infarctions (heart attacks) discover new meaning to their lives and reconnect with their partner, but others see it as a threat to their well-ordered existence.
Researchers from Switzerland and the United States explored the experiences of 24 couples to see whether the one of them having had a heart attack changed their lives and their relationships. According to the researchers, three distinct behavioral patterns emerged as people tried to cope with a person’s heart attack:
Some said that the heart attack was an important and necessary event which had brought them closer together and transformed their lives.
Others felt fearful and threatened by the fact that they had no control over an unpredictable future.
The last group looked at various possibilities for positive change as a result of the heart attack. But they did not achieve them and felt that they had missed their chance to make things better.
It would be easy to pass off the people in the first group with the positive responses as “rationalizers:” people who are trying to make the best of a bad situation. But that would be a mistake. Severe, particularly life-threatening illness can often have a transformative effect on people an those around them. The key is to provide them with positive psychological and spiritual support.
This research strongly reaffirms the principle that successful recovery from a serious illness means more than eradicating it. It really means dealing not just with the physical, but also the psychological, social, subtle and spiritual aspects of what has happened.
In a cardiac rehabilitation program, if a person is in a stable relationship, it is essential to involve both partners in the program so that support can be tailored to their own individual relationship.
The lead researcher was Dr Romy Mahrer-Imhof, from the Institute of Nursing at the University of Basel in Switzerland, and she had this to say, “For example, counseling could provide these couples with more choices about how to negotiate more intimacy in a relationship in which each partner’s needs and wants are respected…. Group session are also useful as they show people how other couples deal with similar situations, helping them to conquer fear and find new ways of living, despite the illness.”
One of the reasons that I’m so militant about aggressive rehabilitation and involving the family is this. As a very young freshly minted doctor, I was involved in the care of a man who suffered from a very small heart attack at the unusually early age of 28. He made an uneventful physical recovery, but announced to his family that he would never work again, and that sexual intimacy or any other kind of physical activity was now out of the question for him. Overnight, he had become a needless cardiac cripple. As he left the hospital he refused to get dressed in regular clothes, but instead wore pajamas and a bathrobe. He shuffled along like an old man despite the fact that his exercise tolerance was probably as good as mine. He refused all offers of help, would not go to rehabilitation and refused to see a psychologist or counselor. Despite the fact that his heart had recovered completely, he died within a year.
Nobody could have forced him into having treatment, and as a newly qualified doctor I was only the team tadpole.
But if I’d known then what I know now, I doubt that he would have had such a sad outcome.
Enabling the re-integration of the whole person – body, mind, spirit, subtle systems and relationships – is the central core of Integrated Medicine and Healing, Meaning and Purpose.
“No man is an Island, entire of it self; every man is a piece of the Continent, a part of the main; if a clod be washed away by the sea, Europe is the less, as well as if a promontory were, as well as if a manor of thy friends or of thine own were; any man’s death diminishes me, because I am involved in Mankind; And therefore never send to know for whom the bell tolls; It tolls for thee.”
–John Donne (English Metaphysical Poet and Divine, 1572-1631)
“Deep within himself man seeks meaning for his life, and tries to fulfill himself in accordance with that meaning.”
–Viktor Frankl (Austrian Psychiatrist and Holocaust Survivor, 1905-1997)
“When we are motivated by goals that have deep meaning, by dreams that need completion, by pure love that needs expressing, then we truly live.”
–Greg Anderson (American Author and Founder of the Cancer Conquerors Foundation, 1947-)
“Love is the ultimate meaning of everything around us”
— Rabindranath Tagore (Indian Poet, Playwright, Essayist, Painter and, in 1913, Winner of the Nobel Prize for Literature, 1861-1941)
Meditation for the Failing Heart
There is a remarkable study in the current issue of the journal Ethnicity and Disease that seems to show that Transcendental Meditation significantly decreases the severity of congestive heart failure.
Researchers from the University of Pennsylvania evaluated 23 African American men and women with an average age of 64 years, who had recently been hospitalized with New York Heart Association Functional Class II or III congestive heart failure. Participants were randomized to either the Transcendental Meditation (TM) technique or health education, in addition to usual medical care.
The investigators used a standard battery of tests to measure changes in heart function with a six-minute walk test, and scales to evaluate quality of life, depression, and re-hospitalizations. They analyzed changes in outcomes from baseline to three and six months after treatment.
The TM group improved significantly on the six-minute walk test after both three and six months of TM practice compared with the control group. The TM group also showed improvements in quality of life measurements, depression, and they had fewer re-hospitalizations.
Congestive heart failure is a serious illness carrying a very significant morbidity and mortality. According to the American Heart Association, congestive heart failure accounts for more than 2.5 million hospital admissions per year in the U.S. Each year, nearly 500,000 new patients are diagnosed with congestive heart failure – and 300,000 patients die annually from this disease. Despite advances in treatment, the number of deaths from congestive heart failure increased steadily over the past decade.
African Americans have twice the mortality rates from congestive heart failure as white Americans.
It is most likely that TM improves the functioning of the heart by reducing the stress associated activation of the sympathetic nervous system that is known to contribute to the failing heart.
The study was sponsored by the National Institutes of Health – National Center for Complementary and Alternative Medicine (NIH-NCCAM) in a collaboration between the University of Pennsylvania with the Institute for Natural Medicine and Prevention at Maharishi University of Management.
“Meditation is the tongue of the soul and the language of our spirit.”
–Jeremy Taylor (English Anglican Clergyman, Writer and Bishop, 1613-1667)
"The purpose of meditation is not enlightenment, it is to pay attention even at extraordinary times, to be of the present, nothing-but-in-the-present, to bear this mindfulness of now into each event of ordinary life.”
–Peter Matthiessen (American Naturalist and Writer, 1927-)
Air Pollution and Cardiovascular Disease

There a very important piece of research published in this week’s issue of the prestigious New England Journal of Medicine, indicating that air pollution increases the risk of cardiovascular disease, at least in women. The whole article is available for free download.
Researchers from the University of Washington studied 65,893 postmenopausal women without previous cardiovascular disease in 36 U.S. metropolitan areas from 1994 to 1998, with a median follow-up of 6 years. All the participants were aged 50 to 79 and part of the Women’s Health Initiative, a major US Government funded investigation into the causes of heart disease in women. A total of 1,816 women suffered one or more cardiovascular event.
The investigators were particularly interested in tiny airborne particles called particulates, which are less than 2.5 microns across, and can lodge in the lungs. Previous research had incriminated them in heart disease. These are the dense clouds that you see coming out of chimneys or exhaust pipes. They found that pollution levels varied between four to nearly 20 micrograms per cubic meter.
Each 10 microgram rise was matched by a 76% rise in the chances of dying from heart disease or stroke. For women living within, rather than between, cities, the risk more than doubled, increasing by 128%, with each step up in pollution levels.
It is not clear whether women are more susceptible to pollution than men. Women’s coronary arteries are smaller and this might render them more vulnerable.
These results suggest that the risk from air pollution is far greater than most doctors previously thought, though it is still not clear how these sooty particles lead to the development of heart disease.
I live just outside a city where we often have smog advisories for weeks at a time in the summer. This research adds to the growing evidence that air pollution should be taken seriously as a risk factor for cardiovascular disease.
That also means that when localized air pollution is particularly high, people with chronic lung disease or coronary heart disease should avoid staying outside.
This problem will likely get worse as the summers be progressively warmer.
Yet another reason for taking climate change seriously.
“For the first time in the history of the world, every human being is now subjected to contact with dangerous chemicals, from the moment of conception until death.”
–Rachel Carson (American Biologist and Writer, 1907-1964)
Tea and Milk

Growing up in England, tea is a great deal more than a drink.
Always drunk hot, of course. No normal person would want it served cold.
It is a major social lubricant and is considered by most to be a separate food group. And the health benefits conferred by a nice cup of tea are now known to just about everyone in Britain.
But from an early age I knew that one day I would have to leave the country.
Why?
Because I could never abide the way in which the vast majority of tea drunk in England is destroyed by the addition of milk and sugar. There are even long technical debates about whether to add the milk before pouring in the tea or after? How fast to add the white stuff? How to stir it in?
Since I was knee high to a puppy I was always the odd one out, wanting nothing to do with this wanton destruction of a sublime beverage.
Which should always be enjoyed au naturel. The only thing that might ever sully a cup of fine Earl Grey or Darjeeling might be a little lemon. Anything else?
Yuk.
Well, it now transpires that this isn’t just a matter of taste buds.
A study just published in the European Heart Journal says it all in the title, “Addition of milk prevents vascular protective effects of tea.”
Tests on sixteen healthy postmenopausal female volunteers showed that black tea significantly improved the ability of the arteries to relax and expand, but adding milk completely blunts the effect. The research was supplemented by tests on rat blood vessels. Tea caused the muscle in the vessel wall to relax by producing nitric oxide from the endothelial cells that line blood vessels. Adding milk blocked the production of nitric oxide and the relaxation of the muscles.
Now bear in mind that they were testing black tea. The researchers are now looking at the potentially more potent green tea to see whether its effects are also blocked by milk.
The villain of the piece is a group of proteins called caseins, which they found interacted with the tea to decrease the concentration of catechins in the beverage. Catechins are the flavonoids in tea that mainly contribute to its protection against cardiovascular disease.
The moral of the story? Tea can be wonderful on so many levels. Not only does it taste good, but also it can do wonders for your health.
But please, please, please don’t lose all the benefits by sloshing in a load of milk!
Raw, naked tea is the way to go…
“Thank God for tea! What would the world do without tea? How did it exist? I am glad I was not born before tea.”
–Sydney Smith (English Clergyman and Essayist, 1771-1845)







