A New Treatment for Parkinson’s Disease?

It is remarkable how often we find that a treatment for one problem may turn out to help something completely different.
Parkinson’s disease is caused by a loss of dopamine neurons in specific circuits in the brain. Dopamine has a great many actions, but I these particular circuits it is involved in the control of movement. Once it starts, the process usually continues on inexorably. The mystery has been why the neurons die in the first place.
There is a very promising article that was published online today in the journal Nature.
Investigators from the Department of Physiology in the Feinberg School of Medicine at Northwestern University in Chicago and the Department of Cellular and Molecular Pharmacology at the Chicago Medical School, Rosalind Franklin University of Medicine and Science have looked at a medicine that is usually used for treating hypertension, and found that it may protect dopaminergic neurons.
Their studies have suggested that the dopaminergic neurons involved are unusually reliant on a type of calcium channel that maintains their rhythmic activity. If the pacemaker is damaged, the neurons become more vulnerable to stressors such as neurotoxins. As we age, calcium ions begin to enter the neurons and change their behavior. They showed that mice that had been engineered to develop a progressive Parkinson’s-type disease did not become ill when their condition was treated with the calcium channel blocker israpidine. Their dopamine neurons appeared to revert back to their original, youthful form.
It is much to early to think about using isradipine for treatment. We do not, for example, know whether it works in humans and we have any idea how much of the drug would be needed. But this research does suggest a whole new line of research and possibilities for treatment.
That is exciting, though when I read about research like this I always wish that researchers did not use animals in their experiments. But since the animals have made the sacrifice to help us, we need to acknowledge their help.
A Major Breakthrough in Neurogenesis Research
I have written a lot about adult neurogenesis, because it is so incredibly important.
When most of us were in school were taught that the brain is a static structure. That you are born with a certain number of neurons, that constitutes your neural “stash.” And after the age of five you would lose a hundred thousand neurons a day, and if you drank too many martinis it would be two hundred thousand a day. “Facts” and figures repeated from one textbook to another for fifty years. And quite wrong.
Ten years ago it was discovered that there are neural stem cells in the hippocampi of adult rodents. A study published in 1998 provided some evidence that neurogenesis takes place in the adult human hippocampus, but the idea that neurogenesis takes place in adult humans has remained contentious.
Now, an advance online publication on the website of the journal Science provides evidence that neurogenesis may also occur in the olfactory bulb of the human brain.
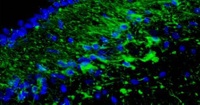
The whole article, including the pictures is available here. The picture at the top of this article shows new cells appearing in the olfactor bulb.
The investigators examined the rostral migratory stream (RMS) which is the main pathway by which newly born cells from the subventricular zone (SVZ) reach the olfactory bulb in rodents. The researchers discovered that there is a human RMS containing neuroblasts, a.k.a. neural stem cells.
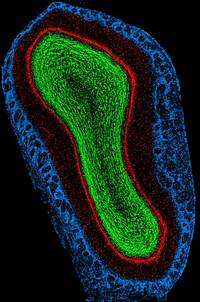
(This is a rat olfactory bulb)
Maurice Curtis and his colleagues examined the brains of cancer patients who had recently died, after having been previously injected with bromodeoxyuridine (BrdU), a chemical that is incorporated into newly synthesized DNA. Cell biologists and oncologists have used the method for years to visualize and monitor the growth of tumors. The researchers found BrdU-positive cells in the olfactory bulbs of the patients’ brains, indicating that they contained newly-generated neurons.
The team then used antibody staining to show that the neuroblasts begin to differentiate into olfactory neurons while migrating through the rostral migratory stream. Upon arriving at the bulb, the cells continued to differentiate, forming mature olfactory neurons.
The patients whose brains were examined were between 38-70 years of age, so the findings show that neurogenesis may occur throughout the duration of the human lifespan. The function of these newly generated cells is unclear, but they may be involved in recognizing and remembering new smells in the later years of life.
The researchers also have preliminary unpublished data that the stem cells not only migrate to the olfactory bulb, but also leave the RMS and migrate into the basal ganglia and cerebral cortex. This is significant, because parts of the basal ganglia degenerate in movement disorders such as Parkinson’s Disease, and specific regions of the cortex degenerate in Alzheimer’s. The possibility that stem cells enter these regions from the RMS could therefore provide a means for developing new treatments for neurodegenerative diseases.
So although at the moment new neurons are only known to be created in a small number of ancient structures in the brain, but that may well change, since the cells are marching over there from regions around the ventricles. After all, why would Nature, the Universe or God have left neural stem cells sitting there unless it was for a good reason? And if adult neurogenesis can be demonstrated in other parts of the brain, then what? An end to the stem cell debates? If the stem cells are already present in the brain, the effort can be directed toward activating and directing them. Could we continue generating new neurons to stave off the dementing illnesses, or is that just science fiction?
The answer is that science fiction is fast becoming science fact. This research will need to be replicated, but I know of several other labs that have already accumulated some similar data to this new paper in Science.
Acupuncture and Parkinson's Disease
Over the last 25 years I have used acupuncture to try and help a great many people with Parkinson’s disease. It has certainly helped a lot of the symptoms, but in my experience has not often done much to change the course of the illness. That being said, I have seen a few people who had remarkable improvements that were sustained for months and even years. The best results have usually come when we have used a combination of acupuncture, diet and homeopathy, in addition to regular medications.
So I was very interested to see a study in the journal Brain Research, even though the work used animals, and I’ve had a longstanding aversion to animal experiments.
There is a chemical called MPTP (1-methyl 4-phenyl 1,2,3,6-tetrahydropyridine) that damages and kills some types of dopaminergic neurons in the brain, so it can produce Parkinsonian symptoms in humans and in some animals.
Mice were injected with MPTP and then some of them received acupuncture every two days in two spots, one behind the knee and one on top of the foot. In humans, these are two of the points that are traditionally considered to be involved in muscle movement. Another group of mice received acupuncture in two spots on the hips that are not believed to be effective for acupuncture. A third group had no acupuncture at all.
By the end of seven days, the MPTP injections had decreased dopamine levels both in the mice that had not received acupuncture, and in the mice that received fake acupuncture, to about half the normal amount. But in the acupuncture-treated group, dopamine levels declined much less steeply, and nearly 80% of the dopamine remained.
The mechanism for such an effect remains unknown. The most likely mechanism is that it is reducing the inflammation in the brain often accompanies and worsens other symptoms of Parkinson’s disease. So acupuncture might maintain dopamine levels by preventing this inflammation. The same team of researchers from South Korea has already reported that acupuncture also prevents loss of dopamine neurons in rats.
The clinical studies in humans have been less encouraging, and more closely reflect my clinical experience. The problem is that by the time most people get to see an acupuncturist, they have already lost huge numbers of dopamine neurons and it is difficult to do very much. If acupuncture is to be helpful, we would probably need to be able to identify someone with Parkinson’s disease extremely early, perhaps even before clinical signs have appeared, and so far we have no reliable way of doing that.
Parkinson's Disease, the Intestine and Infections
Early in my career, one of my mentors was the eminent scientist and clinician Robert Mahler. He recently passed away at the age of 81, but in the last two years of his life he was an author on two papers (1, 2) about an ailment with which he struggled for many years: Parkinson’s disease.
Despite the best treatment, he was severely incapacitated by the illness, at one stage needing a wheelchair to get from his car to his office. But his fine mind remained undimmed by the illness, and he was intrigued by reports of an association between stomach ulcers and Parkinson’s disease and of dramatic improvements in the symptoms of some people with Parkinson’s disease who were being treated with antibiotics for gastric ulcers. (Last year Barry Marshall and Robin Warren were awarded the Nobel Prize in Physiology or Medicine for their pioneering work on Helicobacter – a bacterium associated with peptic ulcers.
I mentioned in an earlier post that I have a strong sense that there are more prizes to come on the
interaction between infectious agents, inflammation, genes, the psyche
and the environment.)
Robert was one of the test subjects in a research study and his Parkinsonian symptoms got much better when he was treated with antibiotics. There are now several important pieces of research on the fascinating topic. In some people eradicating Helicobacter may convert rapidly progressive Parkinsonism to a quieter disease, although only a minority of sufferers have evidence of current infection.
There seems to be an interaction between aging, genes and this infectious agent. Clearly not everyone is helped by antibiotic treatment, but this is a whole new line of very promising research.
Genes, Environment and the Brain

We recently looked at the worrying suggestion that environmental toxins could, in susceptible individuals, be contributing to the apparent increase in autism over the last three decades.
There is increasing evidence that there are complex genetic and environmental interactions that contribute to abnormal aging and neurodegenerative disorders like Alzheimer’s, Parkinson’s and Huntington’s diseases.
A new study from Duke University Medical Center in Durham, North Carolina, has done more to dissect this interaction. They collected information on 1136 consecutive patients who presented to the Joseph and Kathleen Bryan Alzheimer Disease Research Center. They showed possible significant contributions of toxic environmental and occupational exposures to pathological aging in 21% of the patients, and interactions of these exposures with common genetic polymorphisms that affect cell injury and inflammation. They found a series of genes that could partially account for differences in the type of cognitive problems that people experience, the age at which they developed them as well as the rate of progression.
The researchers targeted three genes in particular – apolipoprotein E, alpha-1-antitrypsin and the hemochromatosis gene. All three are expressed in the liver and in macrophages: cells that play a critical role in immune responses, inflammation and the body’s response to stress and infections. The first two genes are particularly involved in the metabolism of lipids and the third in the balance of iron and trace minerals. This ties in with another observation. Many chronic illnesses are associated with anemia. It is now thought that this also is a defensive reaction. Not to chronic illness, but to the problem that was far more common during evolution, and that was infection. The liver pulls iron out of the circulation so that bacteria cannot use it for their own growth. This is one of a number of adaptive responses that I discuss in the book and CD series, Healing, Meaning and Purpose.
But it was also clear form this new study that genes were not the only factor. I have spoken before about the small number of strategies that can dramatically reduce our risk of developing Alzheimer’s disease. The authors of this study agree about the importance of factoring in environmental factors including, alcohol use, nutritional deficiencies and sleep and mood disorders, all of which can have an impact on cognition.
This study is yet another step toward clarifying the role of genes, inflammation and cell injury in the development of degenerative changes in the brain.
While pharmacologists can use this information to help devise new ways to protect your brain, you can use it immediately. There is a range of behavioral and dietary strategies that can reduce the burden of inflammation in the body. I shall write about some of them in articles and an eBook in the near future.
We do not know whether these strategies can reduce the risk of Alzheimer’s and Parkinson’s diseases, but there are some intriguing suggestions that they can.
Pramipexole
Pramipexole is a remarkably interesting medicine about which you are likely to hear a lot in the near future. It is an agonist, which means that it has a positive effect, on D2 dopamine receptors and also on a little-known group of dopamine receptors, known as the D3 group. If you want to get really clever the dopamine receptor D3 group is abbreviated to DRD3. Pramipexole has been in use for almost a decade in the treatment of Parkinson’s disease, and approximately 9.1 million prescriptions for pramipexole have been written in the U.S. since its launch in 1997. It is not without its problems. In Parkinson’s disease it may cause dizziness, involuntary movement, hallucinations, headache, difficulty falling asleep, sleepiness, and nausea. Some people have also had behavioral dyscontrol while taking it.
At a meeting in Athens in February of 2006, we saw confirmation of something that had been shown in previous research: pramipexole seems to be a very effective treatment for restless legs syndrome (RLS). A study published in the journal Neurology has given us a more detailed understanding of the risks and benefits of pramipexole.
The investigators report a 12-week, multicenter, double-blind, randomized, placebo-controlled study of fixed daily doses of pramipexole (0.25 mg, 0.50 mg, and 0.75 mg) involving 344 patients with moderate to severe RLS. Data from 339 patients were analyzed to evaluate the effect of pramipexole treatment on efficacy and safety. The mean age of patients was 51.4 years and the mean duration of RLS symptoms was 5.1 years. The results were very promising, even though half of the patients on placebo also showed an improvement. The most commonly reported side effect included nausea (19.0%), headache (17.8%), insomnia (10.5%) and somnolence (10.1%).
In Europe pramipexole it has been approved for use in this indication. It is marketed as Sifrol® / Mirapexin® In the United States we currently only have one approved medical treatment for RLS, and that is the GlaxoSmithKline medicine ropinirole (Requip), that works at the same D3 receptors in the brain and spinal cord. Ropinirole is effective in a proportion of people with RLS, but it has also been linked to sleepiness, drops in blood pressure and fainting, so those are included in its label.
RLS may be associated with some other illnesses so I was very interested to see two reports of the use of pramipexole in bipolar depression as well as a report of its possible use in REM Behavior Sleep Disorder.
One of the most exciting potential uses for pramipexole may be in some people with fibromyalgia. I’ve mentioned that fibromyalgia, bipolar disorder and some other psychiatric illnesses may be connected. The idea that we might be able to use just one medicine to support our Integrated Medicine approach is very attractive, and also helps point us toward a deeper understanding of what exactly goes wrong at the physical level in RLS, depression and fibromyalgia.
I’ll keep you posted.
Restless Legs Syndrome
Restless legs syndrome (RLS) is a common (3-15% of the population) and sometimes very unpleasant problem in which people have uncontrollable urges to move their legs. If they do not move, they will begin to feel uncomfortable, painful or odd sensations in their legs, and sometimes also in other parts of the body. The restlessness may last for minutes or even hours. Movement affords people very temporary relief. The sensations are usually between the ankle and the knees, but they can also involve the thighs. If other parts of the body are involved it always makes us question the diagnosis.
The severity of the problem is highly variable, running from a mild annoyance to an incapacitating problem. In most people the symptoms are worse when sitting or at night, and often lead to loss of sleep. Not surprisingly many people feel of exhausted and irritable during the day.
With such enormous variations in the severity of the problem, and even the parts of the legs affected, it is highly likely that RLS is a symptom of a group of illnesses.
The International Restless Legs Syndrome Study Group (IRLSSG) identified four criteria that must be present for an RLS diagnosis:
- An urge to move, usually due to uncomfortable sensations that occur primarily in the legs.
- Motor restlessness, expressed as activity, that relieves the urge to move.
- Worsening of symptoms by relaxation.
- Variability over the course of the day-night cycle, with symptoms worse in the evening and early in the night.
About 80% of the people with restless legs syndrome also suffer from a separate condition called periodic limb movements in sleep (PLMS). Periodic limb movements in sleep are involuntary jerking movements in extremities, usually the legs. You can have PLMS without having RLS, and vice versa.
RLS may start at any age, including early childhood, and is a progressive disease for a certain percentage of sufferers, although it has been known for the symptoms to disappear permanently in some sufferers. The condition runs in families; children of RLS sufferers are more likely than other people to develop RLS.
It has some similarities to a syndrome known as akathisia that occurs in people taking some medications that work in the dopamine pathways of the brain. There are some subtle ways of telling the two apart, but RLS also seems to be caused by disturbances in one of the dopamine pathways of the brain.
It has been known for many years that there is an association between RLS and iron deficiency, but this link is probably not causal: just giving iron only helps a proportion of sufferers. But because of this link, everyone with RLS should have their ferritin levels tested; ferritin levels should be at least 75 mcg for those with RLS. If it’s below this level, iron supplements may help, but they are best administered by a physician, because ferritin needs to be monitored and there are down sides to taking too much iron. In a moment I’ll tell you about some very new research on iron and RLS
Caffeine and other stimulants usually make RLS worse. Restless legs syndrome frequently occurs during pregnancy. About 15% of pregnant women develop RLS symptoms during the last few months of their pregnancy. The sensations usually stop after the woman delivers the baby.
We normally divide RLS into primary and secondary. Primary RLS usually starts before age 40 and the onset is often slow. The RLS may disappear for months, or even years. But it can be progressive and get worse as the person ages.
Secondary RLS often had a sudden onset and may be daily from the very beginning. Apart from pregnancy, secondary RLS is a result of a number of medical conditions, so it is always important to rule them out. They include:
- Iron deficiency anemia
- Macrocytic anemia due to folate or vitamin B12 deficiency
- Diabetes mellitus
- Peripheral neuropathy
- Alcohol abuse
- Some types of cancer, particularly of the lung
- Celiac disease
- Renal failure
- Inflammatory arthritis
There have been reports of associations of RLS with other illnesses, but most seem rare. Interestingly people who undergo surgery often find that RLS symptoms become worse, which may be another clue as to the cause of the problem.
An international conference entitled SLEEP 2006, the 20th Anniversary Meeting of the Associated Professional Sleep Societies took place from June 17-22, 2006 in Salt Lake City, Utah. There were a great many interesting papers this year, including several on RLS
An international group of collaborators presented the results of the first population-based pediatric RLS survey. They used the National Institutes of Health pediatric RLS diagnostic criteria and collected data from over 10,000 families. The criteria for definite RLS were met in 1.9% of 8- to 11-year-olds and in 2% of 12- to 17-year-olds. Two different papers explored the value of using a single screening question to identify possible RLS patients. Those who answered, “Yes,” then answered more detailed questions to determine whether they met the International RLS Study Group diagnostic criteria.
A single screening question can eliminate people without RLS rapidly and direct appropriate subjects to further evaluation. Two groups of researchers found a high level of sensitivity with the question, "When you try to relax in the evening or sleep at night, do you ever have unpleasant, restless feelings that can be relieved by walking or movement?"
As I mentioned, it has been known for decades that RLS may be associated with low iron, and especially with low ferritin levels. These may be present in symptomatic RLS patients during pregnancy and in people with iron-deficiency anemia and end-stage renal disease. Previous studies had suggested that supplemental iron was beneficial for RLS patients with low ferritin levels. One paper presented further evidence of the possible efficacy of supplemental iron in the treatment of selected RLS patients with a prospective, randomized, placebo-controlled, double-blind study of RLS patients with low to normal ferritin levels (15-75 mcg/L). The RLS subjects were given either placebo or iron 325 mg twice daily and were monitored with a validated RLS symptom scale. The preliminary findings showed that the iron supplementation group had significant increases in their ferritin levels and had improved quality of life compared with those on placebo; however, the interim data presented did not show a significant change in the RLS symptom score. The study is ongoing.
Treatment for RLS is based on how disruptive the symptoms are. Apart from iron, people should review their lifestyle and see what changes could be made to reduce or eliminate their RLS symptoms. These include: Finding the right level of exercise (too much worsens it, too little may trigger it)
Eliminating caffeine
Stopping smoking
Reducing alcohol intake
Several drugs have been tried for RLS: Some of the same medications used in Parkinson’s disease, benzodiazepines, anticonvulsants like carbamazepine and gabapentin.
Last month saw the publication of an important paper indicating that the medicine pramipexole, another anti-Parkinsonan drug, helps many people with RLS
In the next article I shall review some of the other approaches used by Integrated Medicine.
Aging, Skin and Cancer
There’s a very interesting paper in this month’s issue of the journal Developmental Cell, based on research conducted at the Oregon Health & Science University in Portland, Baylor College of Medicine in Houston and Leiden in the Netherlands.
The investigators have found a pathway through which a gene’s over-expression causes stem cells in the skin to switch from creating hair follicles to creating sebaceous glands. This discovery may not only provide us with new ways of treating hair loss and oily skin, but it may help us to prevent and treat some cancers.
Skin cells turn over very quickly: just think how fast a graze gets covered over. Epidermal stem cells give rise to the outer layer of the skin that serves as a barrier for the body, as well as generating the follicles that produce hairs and sebaceous glands. These glands produce oils to lubricate the skin. In aged skin, a protein called Smad7 is overproduced, which triggers hair loss and sebaceous gland growth.
This is the first study definitively to link Smad7 over-expression and the pathological changes that occur in aged skin.
Here’s the twist: Smad7 shuts down signaling of another group of genes called Wnt. It binds to a Wnt signaling protein known as Beta-catenin and degrades it with an enzyme called Smurf2. (I don’t known why they decided to call it’s call it Smurf: it looks like ponderous chemical humor to me!) Wnt signaling is critical for organ development, but if Wnt signaling is too active, it also causes cancer.
Enhanced Beta-catenin signaling contributes to many types of cancer, including colon, lung and brain. Perhaps inducing over-expression of Smad7 or delivery of Smad7 directly to tumor cells would provide a therapeutic approach because of the boost in Beta-catenin degradation.
And finally, impaired Beta-catenin signaling contributes to neurodegeneration, such as that found in Alzheimer’s and Parkinson’s diseases, retinal degeneration, some bone density defects and aging. For these diseases, blocking Smad7-mediated Beta-catenin degradation may offer a therapeutic approach.
Parkinson’s Disease, Allergies and Inflammation
The symptoms of Parkinson’s disease have been reported throughout history, but it was first described in the modern era by the great Scottish neurologist James Parkinson in 1817. Even after all these years, we still do not know all that much about what causes it. There’s an interesting study in the August issue of the journal Neurology, which is the official publication of the American Academy of Neurology.
Investigators from the Mayo Clinic used what is known as a case-control design (196 cases and 196 matched controls). What they found was that people who suffered from hay fever or allergic rhinitis, are 2.9 times more likely to develop Parkinson’s disease over a 20-year period.
The researchers did not find any association with autoimmune illnesses such as lupus, rheumatoid arthritis, pernicious anemia or vitiligo. They also did not find any association with asthma.
In addition, people who developed Parkinson’s disease used anti-inflammatory agents less frequently than controls, although this result was not statistically significant. The results may support the hypothesis that there is an inflammatory component in the causation of Parkinson’s disease.
You may ask, “Why on earth would anyone even look at a link like this?” The answer is that there have been previous reports of an association between the use of non-steroidal anti-inflammatories and lower rates of Parkinson’s disease in men but not in women and Alzheimer’s diseases.
This study does not suggest that hay fever causes Parkinson’s disease: it provides evidence for an association between the two. Parkinson’s is probably a group of illnesses with different causes. However, if chronic inflammation around the upper airways could produce inflammation in the brain, we might have a whole new way of preventing a degenerative brain disease.
In a future posting I’ll talk about some natural methods for reducing the burden of inflammation in your body.






