Blood Pressure and the Brain

We have known for almost a century that regions of the brain are involved in the control of blood pressure.
Yet over the last three decades most of the emphasis in research into hypertension (high blood pressure) has focused on blood vessels, the heart and kidneys.
Now research from Bristol University in England has been published in this month’s issue of the journal Hypertension, and it may put the brain back into the center of research into the causes and treatment of high blood pressure.
Working with rats, the researchers isolated a protein called JAM-1 (junctional adhesion molecule-1), that is located in the walls of blood vessels in the brain. It appears to trap white blood cells causing obstruction of blood flow in some of the smallest blood vessels. This can cause inflammation and result in poor oxygen supply to the brain, which may in turn trigger events that raise blood pressure.
Though this work is in its early stages, this is exciting stuff: if confirmed, it might be possible to treat hypertension with drugs that reduce blood vessel inflammation and increase blood flow within the brain.
It also ties in with other recent research from Imperial College, London and Oxford University, in which a team of neurosurgeons and physiologists discovered changes in blood pressure while fitting brain electrodes to 15 patients for pain control.
Deep brain stimulation involves placing very thin electrodes on very exact locations in the brain and is already used to relieve pain and to help Parkinson’s disease patients with their movement.
The researchers found that they could make patients’ blood pressure increase or decrease by stimulating very specific regions of the brain with the electrodes. Regions that have been associated with blood pressure control in the past. If they stimulated an area deep down in the midbrain called the ventral periventricular/periaqueductal gray matter, blood pressure went down, and if they stimulated the dorsal periventricular/periaqueductal gray matter it went up.
Nobody is suggesting that we should start sticking electrodes in peoples’ brain, but this chance observation may have profound implications, particularly for people who drop their blood pressure too far when they are treated with standard medicines.
These two pieces of research may also help explain why a balanced inflammation–reducing diet and relaxation may both reduce blood pressure.
Schizophrenia, Psychosis and Psychopathy
Ever since the tragedy in Virginia earlier this week, everyone has been trying to second guess what happened. As I said, to the trained eye there is a lot to suggest that he had a psychotic condition, but whether it was schizophrenia, bipolar disorder or psychotic depression is guess work.
One of the things that has been worrying in all the media coverage has not only been the sensationalism that we have seen in some quarters, but the mistakes that reporters – and even some of the "experts" – have made in talking about mental illness. I have heard people constantly mixing up schizophrenia and psychopathy, which is more accurately called antisocial personality disorder. I have even heard an old mistake that I had thought died years ago: that schizophrenia is a "split personality." I think that mistake probably goes back to a misunderstanding of the roots of the term "schizophrenia," and it was perpetuated by Alfred Hitchcock’s movie Psycho in 1960.
Let me just repeat: schizophrenia is NOT a split personality. Neither is it multiple personality disorder. There is even a lot of discussion whether multiple personality disorder, now known as "Dissociative identity disorder" really exists: a discussion for another day.
Because there has been so much confusion, I thought that it would be good to clarify what each of these disorders is.
You can get some of the information from Wikipedia. What has worried me a bit is that some websites have slightly questionable infrmation. Many people know that I do a great deal of advocacy work for the mentally ill, so these notes are from my own lectures.
For reliable back up information, I recommend using Healia.com to search, and you can check out at Wikipedia, Schizophrenia.com, the National Institute of Mental Health website, Medline Plus and the National Alliance for the Mentally Ill.
Psychosis
Psychosis is simply a generic term for a mental illness in which people have a "loss of contact with reality." There are often other symptoms, such as hallucinations, delusional beliefs, disorganized thinking and a lack of insight into the unusual or bizarre nature of his or her behavior. Almost anything that stresses the nervous system enough may lead to psychosis. I have often told students that it is possible to induce psychosis in just about anyone. It is a symptom and not a disease. We sometimes call it the "fever of the nervous system."
Schizophrenia
This is a group of illnesses that describe a mental disorder characterized by impairments in people’s perception or expression of reality
and by significant social or occupational dysfunction. The point is that other people don’t share their view of reality and it is causing suffering. There is always some smart Alec student who says, "But isn’t religion a delusion?" The answer is no, of course it isn’t. Millions of people share the same beliefs. The second piece is also important: is it causing suffering, distress or disability? Many people have ideas that are "different." That does not mean that they are mentally ill. Professionals should not get involved unless the beliefs are causing a problem.
A person
experiencing schizophrenia typically has disorganized thinking, and may experience delusions or hallucinations. In Western cultures these are most commonly auditory hallucinations. Simply having hallucinations does NOT mean that someone is mentally ill. I seem to be one of the few psychiatrists that supports the aims of the Hearing Voices Network. The Network tries to help people who are experiencing hallucinations and to educate the public and professionals that there are many possible reasons for hearing voices and many have nothing to do with mental illness.
One of the most disabling things about the schizophrenic group of illnesses is that they primarily affect cognition, and that is one of the things that can lead to chronic problems with behavior and emotion. For a long time there was a worry that the cognitive problems were a result of being on some of the older medications. But these cognitive problems were identified decades before the introduction of these medicines. Hence the old name of schizophreia: dementia praecox.
The diagnosis is based on self-report and observation. We do not have a laboratory test for these illnesses, but we are finding reproducible changes in the brain and in many genes. The main evidence for the illnesses is still based on their response to treatment.
There has been a lot of discussion about whether we should abandon the term "schizophrenias," since the current diagnostic approach is flawed: many people have psychotic experiences without becoming dsitressed or disabled. Neither can they – or should they – be diagnosed. This gets back to the categorical and dimensional argument that I have talked about before. The second point is that the label "schizophrenia" can be so stigmatizing.
Antisocial Personality Disorder
Antisocial personaity disorder is also referred to as psychopathy, sociopathy or dyssocial personality disorder. It is a condition characterized by lack of empathy or conscience, and poor impulse control or manipulative behaviors. The term originally came from the Greek psyche (meaning soul, breath or mind) and pathos (to suffer). At one time the term was used to describe all mental illness, and that is why there is confusion. It is quite different from psychosis. Psychosis is a chronic or intermittent symptom that comes on at some time in life. Antisocial personality disorder should have been present all the time, even though we cannot formally diagnose it until the age of eighteen. The term "psychopath" is not a good one: it has no precise equivalent in either the DSM-IV-TR or the ICD-10.
Only a minority of diagnosable psychopaths are violent offenders . There has been a lot of discussion about whether the manipulative skills of some of the non-violent psychopaths are valuable in corporate America, the military and academia, because they may bold and often charismatic leaders. The has even been a suggestion that becoming a "psychopath" may be an adaptation to working in a highly competitive
environment: it gets results for both the individual and for their
corporations or countries.
There is a recent book – Snakes in Suits – that does a good job of exploring these ideas.
In summary:
Psychosis = A symptom
Schizophrenia = A group of acute or chronic illnesses in which psychosis is a central feature
Antisocial Personality Disorder = a.k.a. "Psychopathy:" life long personality trait
Genius Genes

I have talked before about the fascinating topic of child prodigies, and the continuing debate about the contributions and interactions of nature and nurture.
There is an important new study published in the journal Behavioral Genetics that should be of interest to anyone interested in thinking, intelligence and optimizing the potential of children.
A team of researchers from Washington University School of Medicine in St. Louis, has gathered the most extensive evidence to date that a gene that activates signaling pathways in the brain influences at least one kind of intelligence. They have confirmed a link between the gene, CHRM2 and performance IQ, that involves a person’s ability to organize thoughts or events logically.
The team found that several variations within the CHRM2 gene could be correlated with slight differences in performance IQ scores, which measure a person’s visual-motor coordination, logical and sequential reasoning, spatial perception and abstract problem solving skills. When people had more than one positive variation in the gene, the improvements in performance IQ were cumulative.
Typical IQ tests also measure verbal skills and typically include many subtests. For this study, subjects took five verbal subtests and four performance subtests, but the genetic variations influenced only performance IQ scores.
The researchers studied DNA gathered as part of the Collaborative Study on the Genetics of Alcoholism (COGA). In this multi-center study, people who have been treated for
alcohol dependence and members of their families provide DNA samples and investigators have isolated DNA regions related to alcohol abuse and
dependence as well as a variety of other outcomes.
Some of the participants in the study also took the Wechsler Adult Intelligence Scale-Revised, a traditional IQ test. Members of 200 families, including more than 2,150 individuals, took the Wechsler test, and those results were matched to differences in individuals’ DNA.
By comparing individual differences embedded in DNA, the team focused on CHRM2, a muscarinic receptor gene on
chromosome 7. The CHRM2 gene activates a multitude of signaling
pathways in the brain involved in learning, memory and other higher
brain functions. The research team does not yet understand how the gene
exerts its effects on intelligence.
Intelligence was one of the first pscyhological factors that attracted the attention of people interested in the interplay of genes and environmental influences. Early studies of adopted children showed that when children grow up away from their biological parents, their IQs are more closely correlated to biological parents, with whom they share genes, than adoptive parents, with whom they share an environment.
But in spite of the association between genes and intelligence, it has been difficult to find specific variations that influence intelligence. The genes identified in the past were those that had profoundly negative effects on intelligence – genes that cause mental retardation, for example. Those that contribute to less dramatic differences have been much harder to isolate.
The St. Louis team is not the first to notice a link between intelligence and the CHRM2 gene. In 2003, a group in Minnesota looked at a single marker in the gene and noted that the variation was related to an increase in IQ. A more recent Dutch study looked at three regions of DNA along the gene and also noticed influences on intelligence. In this new study, however, researchers tested multiple genetic markers.
The lead investigator in St. Louis, Danielle Dick, had this to say,
“This is not a gene FOR intelligence, it’s a gene that’s involved in some kinds of brain processing, and specific alterations in the gene appear to influence IQ. But this single gene isn’t going to be the difference between whether a person is a genius or has below-average intelligence.”
“One way to measure performance IQ may be to ask people to order pictures correctly to tell a story. A simple example might be pictures of a child holding a vase, the vase broken to bits on the floor and the child crying. The person taking the test would have to put those pictures into an order that tells the story of how the child dropped the vase and broke it and then cried.”
“If we look at a single marker, a DNA variation might influence IQ scores between two and four points, depending on which variant a person carries. We did that all up and down the gene and found that the variations had cumulative effects, so that if one person had all of the ‘good’ variations and another all of the ‘bad’ variations, the difference in IQ might be 15 to 20 points. Unfortunately, the numbers of people at those extremes were so small that the finding isn’t statistically significant, but the point is we saw fairly substantial differences in our sample when we combined information across multiple regions of the gene.”
Most experts believe that there are at least 100 genes that could influence intelligence, but it is unlikely that any one gene is going to be the ONE determinant of how smart someone is. After all, IQ itself has very poor predictive value for anything much in life apart from achievement in high school. The many genes involved probably have small, cumulative effects on increasing or decreasing IQ, and the key will be to understand the interaction between environmental influences and these genes. We already know that childhood nutrition, socio-economic status and emotional and cognitive environments have a profound influence on intelligence and achievement. Altogether too many children have all the mental machinery but do not even realize the possibilities open to them.
It is also clear that early influences will have a lot to do with the repertoire of intelligences that a person has. In the book and CD series Healing, Meaning and Purpose I spend some time discussing Howard Gardner’s important concept of multiple intelligences. Many of us have skills in certain domains and it is a terrible mistake to assume that because a child is not very good at logical or verbal tasks, that they are not smart. After all, how many brilliant musicians, computer scientists and entrepreneurs never finished high school or college?
There is clearly more than a gene deciding our intelligence and success at certain activities. The genes may give us the machinery and the fuel, but there are clearly many other factors. I’ve always been a very keen chess player and I once had a friend who was a nationally ranked contract bridge Master. He would destroy most normal mortals at any card game: including me! Even when we played scratch games of contract bridge he would always try to avoid partnering me: he told me that I sucked too badly! 8-(
He also had a hobby: he built and designed all kinds of board games. He used to get upset that whatever the game, if it was played on a board, I almost always won. But here’s the interesting thing: our IQs were virtually identical. But he was murderously good at card games but not at anything involving a board: another refinement of intelligence. I probably did well with board games because I could plan and visualize in three dimensions. My friend had a phenomenal memory for cards that I simply don’t possess.
As the owners of some establishments in Las Vegas once discovered to their glee….
“Intelligence is quickness to apprehend as distinct from ability, which is capacity to act wisely on the thing apprehended.”
–Alfred North Whitehead (English Mathematician and Philosopher, 1861-1947)
“Intelligence is the ability to find and solve problems and create products of value in one’s own culture.”
–Howard Gardner (American Psychologist and Professor at Harvard, 1943-)
“The test of a first-rate intelligence is the ability to hold two opposed ideas at the same time, and still retain the ability to function.”
–F. Scott Fitzgerald (American Writer, 1896-1940)
“To the dull mind all nature is leaden. To the enlightened mind the whole world sparkles and burns.”
–Ralph Waldo Emerson (American Poet and Essayist, 1803-1882)
“It is the sign of a dull mind to dwell upon the cares of the body, to prolong exercise, eating and drinking and other bodily functions. These things are best done by the way; all your attention must be given to the mind.”
–Epictetus (Phrygian-born Greek Stoic Philosopher, c.A.D.55- c.A.D.135)
New Causes for Hope in Psychotic Illnesses
Since many health care providers read this blog, I try to update everyone on promising new treatments that can be used to provide a comprehensive care plan for people.
I have talked before about some new medicines for the treatment of schizophrenic illnesses, and yet more are coming down the road.
There is a short article with quite a number of links here.
"I would like to quote something from the article that is very important for all of us:
It is very interesting that most experts are now focusing on medicines that will make it easier for us to undertake psychosocial rehabilitation, rather than simply relying on a medicine to "cure" the illness.The most important message from all this research is that the future looks promising for many of our sickest patients."
Medicines designed to help and support, not to sedate or damp down the mind’s activity, but to enable a person to take back control of themselves, their thinking and theior emotions.
Teenage Mood Swings

How many of us have been perplexed by the violent mood swings of teenagers? One minute they are out skipping through the countryside and picking wild flowers. The next they seem intent on burning down the forest…
The mood swings and anxiety often make them seem as if they have some kind of “bipolar-lite.”
An important new study has revealed that teenage mood swings may be explained by biological changes in the adolescent brain. The research is published in the journal Nature Neuroscience.
Sheryl Smith, a physiologist at the State University of New York, and her colleagues experimented on adolescent female mice and showed that their brains respond to stress in a different way from adults and pre-pubescent individuals.
Anxiety is highly complex and involves a cascade of chemical neurotransmitters and genes. One of its important regulators is the brain’s principal inhibitory neurotransmitter, gamma-aminobutyric acid (GABA). GABA counteracts the effect of glutamate, an excitatory neurotransmitter in the limbic system of the brain. There is a kind of Yin/Yang relationship between GABA and glutamate.
The brain is full of what are known as “Neurosteroids:” steroid molecules that interact with genes and receptors in nerve cells. Neurosteroids generally reduce anxiety, but this research shows that they promote anxiety in female mice around puberty via the selective desensitization of extrasynaptic GABA-A receptors.
Stress causes the release of a steroid known as 3α,5α-Tetrahydroprogesterone also known as Allopregnanolone or THP. In adult and pre-pubescent individuals THP increases the “calming” effect of GABA in the limbic system. However, Smith and her team found that THP had the opposite effect in adolescent mice. In other words the developing adolescent brain simply behaves differently
It would appear that THP has two roles, one in the limbic system where it helps to calm things down, and another in the hippocampus where in adolescents it heats things up. The hippocampus is important in memory and also in the regulation of emotion.
The underlying mechanism appears to be different levels of expression of a type of receptor known as the “alpha-4-beta-2-delta” GABA-A receptor in the hippocampal brain region known as CA1.
In adults and pre-adolescents there are few of these receptors and THP modulates and calms these regions of the brain.
However, in adolescents, the expression of these receptors is high, and the anxiety raising effect of THP in the hippocampus outweighs the calming effect it has in the limbic system.
Smith and her team were able to reverse the puberty effect in the mice by genetically altering the number of receptors.
The result of all this is that the teenage brain amplifies its reactions to stress. So whether the young person reacts by crying or being angry, the emotion will be much more pronounced than it would be in a pre-pubescent person or an adult. To adults it may seem like an overreaction, to the teenager it is his or her only response.
This study is thought to be the first to suggest an underlying physiological, as opposed to a psychological explanation for teenage mood swings.
Apart from raising understanding about what teenagers are going through, the finding raises the possibility of a new approach to more severe mood swings, such as bipolar disorder.
Madness and Genius Revisited
I must have heard a thousand times that there’s a fine line between genius and insanity. I have talked before about the possible link between the two through schizotypal personality disorder. It is quite well known that there are two living Nobel Prize winners who have a diagnosis of schizophrenia and many more who have first-degree relatives with it.
There is some very interesting research in the current issue of the Journal of Clinical Investigation from a team of scientists at the National Institutes of Health’s (NIH) National Institute of Mental Health (NIMH).
In the latest installment of a story that has been unfolding over the last three decades, they report on their findings concerning a human gene for a master switch in the brain called DARPP-32. Most people inherit a version of a gene that optimizes their brain’s thinking circuitry, yet paradoxically also appears to increase risk for schizophrenia, an illness marked by impaired thinking. The main kinds of thinking involve reasoning, abstraction and creativity.
Over the last two decades, studies in animals, most notably by Nobel Laureate Paul Greengard at Rockefeller University, have established that DARPP-32 in the striatum switches streams of information coming from multiple brain chemical systems so that the cortex can process them. Both the neurotransmitter that DARPP-32 works through – dopamine – and the chromosomal site of the DARPP-32 gene have been implicated in schizophrenia.
The NIMH researchers in this new study have identified a common version of the gene and showed how it impacts the way in which two key brain regions exchange information, so affecting a range of functions from general intelligence to attention.
To understand DARPP-32’s role in the human brain, they used genetic, structural and functional magnetic resonance imaging and also post-mortem studies to identify the human gene’s variants and their functional consequences.
Seventy five percent of subjects had the most common version of the gene, which boosted the activity of circuits in the prefrontal cortex of the brain. This region is the major filter, controller and processor of cognitive information. When active, it increases structural and functional connections and our performance on tasks that involve thinking. It almost certainly does so by increasing gene expression. In 257 affected families, people with schizophrenia were also more likely to have this common version of the DARPP-32 gene.
DARPP-32 appears to shape and control a circuit running between the striatum and prefrontal cortex. The circuit affects key brain functions implicated in schizophrenia, such as motivation, working memory and reward-related learning.
The senior investigator is Daniel Weinberger, who had this to say,
"Our results raise the question of whether a gene variant favored by evolution, that would normally confer advantage, may translate into a disadvantage if the prefrontal cortex is impaired, as in schizophrenia. Normally, enhanced cortex connectivity with the striatum would provide increased flexibility, working memory capacity and executive control. But if other genes and environmental events conspire to render the cortex incapable of handling such information, it could backfire — resulting in the neural equivalent of a superhighway to a dead-end."
Although several groups of researchers have looked for the possible clinical relevance of DARPP-32, they have had much success. This study shows a strong connection between the molecule and human cognition and also, perhaps, with schizophrenia.
What is also interesting about this finding is that it helps provide us with a mechanism by which environmental stress could lead to cognitive problems.
Apart from the uninformed tirades of Tom Cruise, I see a lot of opinion pieces on websites and YouTube expressing the opinion that psychiatry is baseless, ostensibly because there is no science behind it. By anyone’s standards, this is high level science utilizing a series of state-of-the-art approaches. And another piece of evidence that psychiatry is becoming more science than art, linking the mind, the brain and the environment into one harmonious whole.
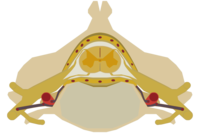
Does the Spinal Cord Think?
In recent years we have become very interested in the ever-increasing evidence there are large complex neural networks outside the brain and autonomic nervous system. The main ones are in the intestine and the heart. These systems are so complex and well organized that some people have talked about us having a “brain” in the heart and another in the intestine. This may be a bit of an over-statement. For instance the cerebellum at the back of the brain is large and highly complex, but is so arranged that it probably cannot generate conscious experience. That particular trick needs a cerebral cortex that self-organizes, recruits new systems when necessary for some particular task and generates vast oscillations that are modulated by genes and the environment.
Now new research has shown that the spinal cord has some of those same properties that we associate with the cerebral cortex. This groundbreaking work has just been published in the journal Science, and the entire paper is available here.
So why the excitement and interest? It often astonishes me how many students who come to my lectures seem not to have a curiosity gene. And there is so much about which we should be curious. Despite the billions spent on research there is still a great deal about the human body that is not understood at all. Not small esoteric things, but huge questions.
For instance how can some people think and communicate even if most of the brain is destroyed by disease? On the other hand some people are incapacitated by the smallest lesion. I’ve taught neurology for years, in particular the art of neurological examination. I was trained by some of the best in the world, so I know how to look for subtle neurological signs. Yet I’ve seen a great many inexplicable things: I saw someone come to autopsy who had no neurological signs, but had a tumor occupying more than half of the dominant hemisphere of the brain.
Here’s another puzzle: we don’t know how humans are able to move. Our muscles are controlled by thousands of nerve cells in the brain, spinal cord and peripheral nervous system. This entire complex system must work as a whole in order to successfully generate a single motion. Yet how quickly do most children learn to stand and walk. The new research has shown that the spinal cord is not a passive signal conductor, but has instead shown that spinal neurons, while engaged in the network activity underlying movements, show irregular firing patterns similar to those seen in the cerebral cortex. Even if we repeat a certain motion with high accuracy, the nerve cells involved never repeat their activity patterns. Just the same as happens in the cerebral cortex.
This is yet more evidence to suggest that “thinking” does not only go on in the brain. It makes sense to think of the major systems – heart, intestine and spine – as key components of the subliminal, pre-conscious mind. Some people like the term subconscious, but that runs into the confusing problem of mixing up the terms subconscious and unconscious.
I talk about some of these differences and how to work these different parts of yourself in the book and CD series Healing, Meaning and Purpose.
Chiropractors have been telling us for years that the spinal cord is a lot more than just a relay system. It looks as if they may have been correct.
If you are interested in following up on my comments about what it takes for a neural network to generate conscious experiences, you may be interested in having a look at my review of the excellent new book Rhythms of the Brain by Gyorgy Buzsáki. and
Daniel J. Benor's WHEE
I have become convinced that the so-called tapping therapies have a great deal to offer many people, as bizarre a they appear the first time that you encounter them!
I have recently come across another form of therapy developed by the holistic psychiatrist and author Daniel J. Benor. I have met Dan many times, and he is one of the most knowledgeable people that I know when it comes to healing, and this new technique seems to be helping a great many people.
He calls it WHEE: Whole Healing – Easily and Effectively, a.k.a. Wholistic Hybrid derived from EMDR and EFT.
Like the other tapping therapies, it seems often to be a quick way to release psychological and physical pains, and it is said to enhance performance in sports. Interestingly, it also seems to help some allergies. There are many helpful resources and a articles at the parent website: Wholistic Healing Research.
If you are looking for more options in your own path toward wellness, or if you have some stubborn problem to deal with, WHEE and the accompanying materials might well be worth your attention.
Back Pain, The Brain and Pain Cycles

A German research team using a specialized imaging technique called diffusion tensor imaging (DTI) to look at the differences between back pain sufferers’ and healthy volunteers’ brains found that individuals suffering from chronic low back pain also had micro-structural changes in their brains. The findings were presented at the annual meeting of the Radiological Society of North America in Chicago by the lead researcher Dr Jurgen Lutz, a radiologist at Ludwig-Maximilians University in Munich, Germany.
DTI tracks the movement of water molecules in the brain’s gray and white matter. Individual water molecules are constantly in motion, colliding with each other and other nearby molecules, causing them to spread out, or diffuse. DTI allows us to analyze water diffusion in the tissues of the brain. In normal white matter, water diffuses in only one direction. So if they are moving in the “wrong” direction, we can use this as an indication that there are changes in the fiber pathways.
The investigators studied 20 patients who were experiencing chronic back pain with no precisely identifiable cause and 20 age- and gender-matched healthy volunteers. DTI was performed to measure the diffusion in several areas of each patient’s brain.
They discovered the brains of patients with chronic back pain had a more complex and active microstructure compared with the healthy volunteers’ brains.
The changes were found in regions of the brain associated with pain-processing, emotion and stress response, including the cingulate gyrus, postcentral gyrus and superior frontal gyrus.
Although it is possible that theses structural disturbances are a cause of chronic pain, it is more likely to be the other way round.
This leads us to a very important concept that is not talked about as much as it should be: it is the idea of pain cycles. Pain cycles can have a physical or psychological origin and are thought to be maintained by some of the centers in the brain that process pain and emotional distress. The two are often mixed together: pain is extremely common in both depression and in bipolar disorder, and pain can, of course, make you feel depressed.
Theses pain cycles will often persist for long periods after the original cause of the pain has gone. So we may continue to feel pain long after a broken bone has healed, or we may continue to suffer emotionally long after a bad relationship should have been dead and buried. Many interventions like acupuncture or injecting steroids or anesthetics into trigger points can interfere with the pain cycle. Similarly there are many therapies, including some of the tapping therapies, that seem to “re-set” some of the systems in the nervous and subtle systems of the body.
In my forthcoming book Sacred Cycles, I talk a lo about these vicious pain cycles and how to interrupt them.
“Pain is part of being alive and we need to learn that. Pain does not last forever, nor is it necessarily unbeatable, and we need to be taught that.”
–Rabbi Harold S. Kushner (American Rabbi Aligned with the Progressive Wing of Conservative Judaism and Writer, 1935-)
“Softness is a dream in every ache to become a better soul.”
–John Kells (Irish-born British Grand Master of T’ai Chi Ch’uan, 1940-)
A Major Breakthrough in Neurogenesis Research
I have written a lot about adult neurogenesis, because it is so incredibly important.
When most of us were in school were taught that the brain is a static structure. That you are born with a certain number of neurons, that constitutes your neural “stash.” And after the age of five you would lose a hundred thousand neurons a day, and if you drank too many martinis it would be two hundred thousand a day. “Facts” and figures repeated from one textbook to another for fifty years. And quite wrong.
Ten years ago it was discovered that there are neural stem cells in the hippocampi of adult rodents. A study published in 1998 provided some evidence that neurogenesis takes place in the adult human hippocampus, but the idea that neurogenesis takes place in adult humans has remained contentious.
Now, an advance online publication on the website of the journal Science provides evidence that neurogenesis may also occur in the olfactory bulb of the human brain.
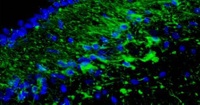
The whole article, including the pictures is available here. The picture at the top of this article shows new cells appearing in the olfactor bulb.
The investigators examined the rostral migratory stream (RMS) which is the main pathway by which newly born cells from the subventricular zone (SVZ) reach the olfactory bulb in rodents. The researchers discovered that there is a human RMS containing neuroblasts, a.k.a. neural stem cells.
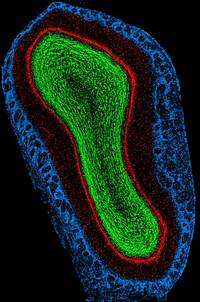
(This is a rat olfactory bulb)
Maurice Curtis and his colleagues examined the brains of cancer patients who had recently died, after having been previously injected with bromodeoxyuridine (BrdU), a chemical that is incorporated into newly synthesized DNA. Cell biologists and oncologists have used the method for years to visualize and monitor the growth of tumors. The researchers found BrdU-positive cells in the olfactory bulbs of the patients’ brains, indicating that they contained newly-generated neurons.
The team then used antibody staining to show that the neuroblasts begin to differentiate into olfactory neurons while migrating through the rostral migratory stream. Upon arriving at the bulb, the cells continued to differentiate, forming mature olfactory neurons.
The patients whose brains were examined were between 38-70 years of age, so the findings show that neurogenesis may occur throughout the duration of the human lifespan. The function of these newly generated cells is unclear, but they may be involved in recognizing and remembering new smells in the later years of life.
The researchers also have preliminary unpublished data that the stem cells not only migrate to the olfactory bulb, but also leave the RMS and migrate into the basal ganglia and cerebral cortex. This is significant, because parts of the basal ganglia degenerate in movement disorders such as Parkinson’s Disease, and specific regions of the cortex degenerate in Alzheimer’s. The possibility that stem cells enter these regions from the RMS could therefore provide a means for developing new treatments for neurodegenerative diseases.
So although at the moment new neurons are only known to be created in a small number of ancient structures in the brain, but that may well change, since the cells are marching over there from regions around the ventricles. After all, why would Nature, the Universe or God have left neural stem cells sitting there unless it was for a good reason? And if adult neurogenesis can be demonstrated in other parts of the brain, then what? An end to the stem cell debates? If the stem cells are already present in the brain, the effort can be directed toward activating and directing them. Could we continue generating new neurons to stave off the dementing illnesses, or is that just science fiction?
The answer is that science fiction is fast becoming science fact. This research will need to be replicated, but I know of several other labs that have already accumulated some similar data to this new paper in Science.






