Brain-Derived Growth Factors and Bipolar Disorder
As we are learning more about the plasticity of the brain, and the way in which new neurons can continue to grow throughout life, there is a great deal of interest in factors that stimulate the growth or development of neurons. This is particularly important in condition like schizophrenia and bipolar in which cognitive decline may occur.
Researchers from Portugal presented some interesting new data (NR68) on Monday at the 2007 Annual Meeting of the American Psychiatric Association in San Diego, California.
Genetic and pharmacological studies have suggested that brain-derived neurotrophic factor (BDNF), one of the most common neurotrophic factors in the brain, may be associated with the pathophysiology of bipolar disorder. The data has been a bit of a mixed bag: previous studies have suggested that BDNF may be associated with either a worse or better neurocognitive outcome in tests of frontal lobe function.
The researchers examined 28 people with bipolar disorder whose mood was currently normal: i.e. they were euthymic, and they compared them with 25 healthy volunteers. They measured BDNF levels and performed a battery of neuropsychological tests.
The people with bipolar disorder had clear evidence of problems with attention and executive function even when their mood was normal. However it does not seem to have much to do with BDNF: the levels were the same in both patients and healthy volunteers. There was an association between BDNF levels and memory in people with bipolar disorder. This makes sense: BDNF has been implicated in the formation of memory traces in the brain.
What this means is that problems of attention and executive function are likely to be trait-markers of bipolar disorder, while BDNF levels may be a state-related biological marker.
It is interesting how the wheel keeps turning: the person who first differentiated dementia praecox (schizophrenia) from manic depression (bipolar disorder) was Emil Kraepelin. He originally said that people with dementia praecox became worse over time, because of progressive cognitive decline, while people with manic depression did not. When he passed away in 1926 he was working on a whole re-visioning of mental illness, saying that the two could not be so clearly differentiated, because cognitive decline could occur in either illness.
Many pharmaceutical companies are looking into the possibility of improving cognition in major mental illnesses, but there are also a great many non-pharmacological interventions that can be done to help cognition in people with major mental illness.
Musical Hallucinations

A paper on auditory hallucinations of music was presented
this afternoon at the 2007 Annual Meeting of the American Psychiatric
Association in San Diego, California.
The researcher looked at 22 people diagnosed with schizophrenia and
23 with schizoaffective disorder at Maimonides Medical Center in
Brooklyn, New York. The question was whether it would be possible to
use the presence of musical hallucinations to distinguish between
schizophrenia and schizoaffective disorder. The conclusions from the
study were that these auditory hallucinations of music were more common
in people with schizoaffective disorder and that voices with a
religious or superstitious content were more common in people with
schizophrenia.
Though it is good to see someone examine the content of hallucinations, this was a very puzzling study.
First, there is always a lot of debate around the “schizoaffective”
diagnosis. Although there are clear criteria for it in the DSM-IV, many
experts believe that most people who have been labeled
“schizoaffective” actually have a form of bipolar disorder. But in any
case, bipolar disorder and schizophrenia probably lie on a spectrum.
People’s diagnoses often change over time. Not because of disagreement
or inaccuracy, but because people change over time. The term
“phenomenological drift” has been used to describe this observation.
What that means is that we always need to be sure of the diagnosis at
the time of the study, rather than what was written in the chart in the dim and distant past.
The other point is that genuine musical hallucinations are very
rare. The world literature contains under a hundred papers in European
languages, and the classic paper,
published by German Berrios in 1991 was an analysis of just 46 cases.
Berrios is regarded by many as one of the finest phenomenologists in
Europe, so it is surprising that the investigator in New York found so
many cases.
It will be good to see if the author or someone else can replicate
the work. The classic teaching about musical hallucinations has been
that they:
- Are more common in women
- Are more common in people who have hearing problems or are deaf
- Are more likely to occur in people with neurological diseases, including Alzheimer’s disease
- If they occur in people with neurological disease, it is more
likely that the damage will be in the right or non-dominant hemisphere
of the brain. (In men, language tends to be in the dominant hemispheres
and music in the non-dominant. The pattern is a bit more complicated in
women, but they also usually sing and recognize music with the right or
non-dominant hemisphere)
A recent report from Japan reported that an elderly man with musical hallucinations was helped with the cholinesterase inhibitor donepezil (Aricept), suggesting that cholinergic neurons are somehow involved in generating musical hallucinations.
Many of us have music or tunes giong round in our heads, but that is quite different from hallucinating music.
And let me repeat: hearing things is common, and does not mean that someone is mentally ill.
Non-pharmacological and Lifestyle Approaches to Attention-Deficit/Hyperactivity Disorder: 6. Biofeedback
It seems odd that hyperkinetic children and adults with attentional problems should be able to stop long enough to try yoga, meditation of biofeedback. Yet there is good evidence that they can and they do, and that all three modalities can be helpful.
Today we are going to look at the use of a specific form of biofeedback.
Neurofeedback is a form of behavioral training that is aimed at developing skills to help people self-regulate the activity of their brains.
The first attempts to use biofeedback in children with behavioral problems took place in the early 1980s, following some interesting work on using it to control epilepsy, headaches and an array of other problems. Several good quality neurofeedback studies have been published over the last ten years.
In neurofeedback training, people are taught to control specific aspects of electrical brain activity. They are hooked up to machine that records electric impulses from the brain – a form of electroencephalograph (EEG) and they are given immediate feedback and positive reinforcement, usually using a visual display.
In frequency training, people are asked to increase or decrease the activity of different EEG frequency bands. To learn to regulate their level of cortical excitability they are trained to generate and regulate slow cortical potentials (SCPs). Slow cortical potentials are slow event-related direct-current shifts of the EEG.
With a little practice, almost anyone can learn the basic techniques, and as they do, they constantly improve their ability to regulate their attention, thoughts, moods and reactions. Many young people with attention-deficit hyperactivity disorder (ADHD) look at it like a game, and quickly become engaged with it.
Studies of neurofeedback have shown some specific effects on attention and memory processes. The key point is that the improvements in performance are maintained once the person is engaged in real-life activities. The techniques can be used to help healthy people perform better as well as helping people with problems.
Several studies have shown that children with ADHD had improvements in behavioral and cognitive variables after both frequency (e.g., theta/beta) training and SCP training. Some of the improvements have been sustained for six months. It has also been possible to show improvements in some neurophysiological measurements. Most studies have been done in children with ADHD, and in most other things were done as well. For instance the children were kept on medications, or children were given other types of exercises to reinforce what they were learning.
There has been some good brain imaging research that has shown that neurofeedback in children with ADHD normalizes the functioning of the anterior cingulate cortex, the key neural substrate of selective attention
There is also another type of feedback training. There is evidence that the level of activity in a classroom containing hyperactive boys can be reduced using feedback about the level of activity together with positive reinforcement. Some recent research has produced preliminary data in which investigators used a device that combines a beeper and actigraphy technology for measuring, monitoring, and modifying motor excess in children. The feedback reduced the activity level of seven out of nine hyperactive boys.
There remain a lot of unanswered questions about biofeedback in the treatment of ADHD. In an excellent review article, John Gruzelier and Tobias Egner from London pointed out that neurofeedback had grown and been widely adopted with little in the way of research to back it up. However their own work has shown that the technique can help improve cognition, and they provided the first evidence of conscious control over the ratio of alpha and theta waves in the brain. They also showed that the technique could lead to remarkable improvements in artistic aspects of music performance, which were equivalent to two class grades in conservatory students.
The evidence for biofeedback is growing, and since it is non-invasive ad may be associated with a number of other improvements in mood and cognition, it will likely bean important option for some people with ADHD.
Genes, Culture and Aging
The study of genetics is becoming ever more interesting. Not only have we gone well beyond the nature/nurture debate, but also there is more and more interest in genetic influences on culture and vice versa: the way in which culture impacts gene expression. It is also clear that our brains are amazingly plastic: nutrition, emotional environment, education and experience all impact brain development.
Now it appears that culture does indeed affect the brain.
Westerners and East Asian people process visual information differently: Westerners preferentially process objects, while Asians tend to pay more attention to contextual information. In studies of semantic organization, Asians associate pictures based on functional relationships, for instance grouping together a mother and her child based on maternal relationship. Westerners based their associations on physical features and categorical membership, such as grouping together a woman and a man because they are adults. These differences may be changing as young people in Asian cultures are becoming more westernized.
New research has found that the aging brain reflects cultural differences in the way that it processes visual information. This study “Age and culture modulate object processing and object-scene binding in the ventral visual area” is published this month in the journal Cognitive, Affective & Behavioral Neuroscience. This paper (which can be downloaded here) and another published by the same group in 2006 are the first to demonstrate that culture can alter the brain’s perceptive mechanisms.
The research is the result of a collaboration between Denise Park’s group from the University of Illinois and Michael W. Chee, of the Cognitive Neuroscience Laboratory, SingHealth, in Singapore. The researchers conducted an array of cognitive tests on study subjects at their facilities in the U.S. and Singapore, and used identical functional Magnetic Resonance Imaging (fMRI) scanners at both sites. Their analysis involved 37 young and old East Asians, and 38 young and old Westerners. They found significant cultural differences in how the older adults’ brains responded to visual stimuli.
As Professor Park said,
“These are the first studies to show that culture is sculpting the brain. The effect is seen not so much in structural changes, but at the level of perception.”
We have known for decades that East Asians and Westerners process visual information differently. A paper in 1972 reported that East Asians are more likely to pay attention to the context and relationships in a picture than are Westerners, who more often notice physical features or groupings of similar subjects.
More recent research, which analyzed the eye movements of East Asians and Westerners viewing identical images, found that Westerners were more attentive to central, or dominant, objects, while East Asians paid more attention to the background, or scene.
Last year the team reported differing patterns of neural activation in the brains of East Asians and Americans shown identical pictures. The Americans showed more activity in brain regions associated with object processing than the East Asians, whose brains showed more activity in areas involved in processing background information.
The new study takes this work further, comparing neural responses to visual stimuli in young and old adults in both cultures. These are some of the pictures they used in the experimenets:
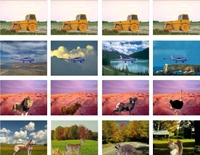
The researchers found that all four groups – young and old East Asians; young and old Americans – processed background information in part of the brain called the parahippocampal gyrus: a region that is vital to memory encoding and retrieval. As expected, older adults in both cultures had less ability to use “binding mechanisms” – the ability to connect a particular object to its background – in the hippocampus. The older people also had diminished object processing in the lateral occipital cortex.
The most striking finding was that the “object areas” of the brains of older East Asian subjects responded much more weakly to novel stimuli than did those same brain regions in the older Americans. For the older East Asians, a lifetime of attention to the backgrounds, or context, of pictures eventually showed up as a diminished response in the part of the brain that keeps track of foreground objects.
One of the best ways of keeping the brain healthy is with cognitive cross training: doing things like crossword puzzles, but also doing things that exercise other cognitive muscles, like playing the piano. This research would suggest that the exact strategies that we should use will be different in native-born Asian and western-born people. Something to factor in the next time that we get some advice about how to keep the brain young for as long as possible.
Risk-taking in Teenagers

The study of adolescence is in an intersting state of flux.
The expectation that teenagers are rebellious by nature is probably not correct. After all, it is nly recently that adolescence, which more or less corresponds to the teen years, has been recognized at all. As recently as the early 1960, most young people went straight from school to employment, and wore the same clothes as everyone else at work. And of course that is still the pattern in many parts of the world, with the exception of school, which is sadly unavailable to so many. In most cultures teenage rebellion is not recognized at all.
Two years ago Professor Philip Graham, author of an excellent book published by Oxford University Press called ‘The End of Adolescence’ and a leading child and adolescent psychiatrist, challenged the myth that teenagers are trouble. He believes that the social attitudes towards the ‘adolescent stereotype’ that prevail in Western society have significant negative effects on the mental health of young people.
This stereotyping can cause some real problems:
- Low expectations of behaviour are often shared by teenagers themselves, leading to low self-esteem
- at least some of the frustration shown by young people in secondary schools can be attributed to the fact that they are ‘disempowered’ in relation to their intellectual and emotional competence
- The legal position of young people, for instance in relation to the age of criminal responsibility, voting age and the consumption of drugs and alcohol, is wildly inconsistent, and results both in injustice and in inadequate preparation for adult life
- The organisation of mental health services often fails to take into account the need to recognise the ‘young adult’ status of this age group.
The other side of this research is the risky behavior of many young people.
There is an excellent review in this month’s issue of Current Directions in Psychological Science by Laurence Steinberg, Distinguished University Professor and the Laura H. Carnell Professor of Psychology at Temple University in Philadelphia. He is also the Director of the John D. and Catherine T. MacArthur Foundation Research Network on Adolescent Development and Juvenile Justice.
The review points out that over the past 10 years there has been a great deal of new research on adolescent brain development that sheds light on why yonug peple engage in risky and dangerous behavior. And also answer the question about why the educational programs or interventions that have been developed have not been especially effective. According to Steinberg, heightened risk taking in adolescence is the result of competition between two very different brain systems, the “socioemotional” and cognitive-control networks. Both are undergoing maturation during adolescence, but along very different timetables. During the adolescence, the socioemotional system becomes more assertive during puberty, while the cognitive-control system gains strength only gradually and over a longer period of time.
The “socioemotional” system processes social and emotional information, and it becomes very active during puberty, allowing adolescents to become more easily aroused and experience more intense emotion. They also become more sensitive to social influence.
On the other side, the cognitive-control system is the part of the brain that regulates behavior and makes the ultimate decisions, but it is still maturing during adolescence and into a person’s mid-20s and perhaps beyond.
The socioemotional system is not always going full bore. When the system is not highly activated, for example, when individuals are not emotionally excited or they are alone, the cognitive-control network is strong enough to impose regulatory control over impulsive and risky behavior, even in early adolescence.
In the presence of peers, or in situations where emotions run high, the socioemotional network becomes sufficiently activated to diminish the regulatory effectiveness of the cognitive-control network.
Steinberg cites a study in which the presence of peers more than doubled the number of risks teenagers took in a video driving game.
As he says,
“In adolescence, not only is more merrier — it is also riskier.”
“There is a window of vulnerability in teens between puberty and mid-to-late adolescence in which kids have already started to experience the increased arousal of the socioemotional system, but they don’t yet have a fully mature cognitive control system,” he says. “Because their cognitive-control system is still not fully mature, it is more easily disrupted, especially when the socioemotional system is quite excited. And it gets excited by the presence of other people.”
“I don’t want people to think that education should not continue, I just think that it alone is not going to make much of a difference in deterring risky behavior. Some things just take time to develop, and, like it or not, mature judgment is probably one of them.”
Steinberg advocates stricter laws and policies that would limit opportunities for immature judgment that often have harmful consequences. For example, strategies such as raising the price of cigarettes, more vigilantly enforcing laws governing the sale of alcohol, expanding adolescents’ access to mental-health and contraceptive services, or raising the driving age would likely be more effective than education in limiting adolescent smoking, substance abuse, pregnancy, and automobile fatalities.
This is controversial stuff, but is also an illustration of a way in which science can help us make better decisions about how best to help young people to avoid auto-destruction.
Neurologically, teenagers are not just small adults, they are still large children. The problem is heightened because so many young people are constantly multi-tasking and children are being exposed to risky behaviors at ever younger ages, when their brains are least able to handle complex decisions about things that may have long-term consequences for them.
Linking Depression, Diabetes and Alzheimer’s Disease

It has been known for many years that Alzheimer’s disease and depression are associated with type 2 diabetes. Good control of blood glucose may reduce the risk of developing Alzheimer’s disease and depression, while treating depression may improve metabolic control.
Decreased levels of brain-derived neurotrophic factor (BDNF) have also been implicated in the pathogenesis of Alzheimer’s disease and depression, and animal models have suggested that BDNF may play a role in insulin resistance.
So a group of scientists at The Centre of Inflammation and Metabolism, Department of Infectious Diseases at the University of Copenhagen in Denmark, decided to see whether BDNF plays a role in human glucose metabolism.
In the first study they looked at 233 people and found that BDNF was inversely associated with fasting plasma glucose, but not with insulin. In a second smaller study they did what are known as hyperglycemic and a hyperinsulinemic-euglycemic clamp studies, that allowed them to look at the relationships between BDNF, glucose and insulin. What they found was that output of BDNF from the brain was inhibited when blood glucose levels were elevated.
So it seems that low levels of BDNF accompany impaired glucose metabolism. Decreased BDNF may be a factor involved not only in dementia and depression, but also in type 2 diabetes, and it may be the missing link that explains the way in which the three conditions cluster together in epidemiological studies
This link between a chemical produced in the brain and diabetes is not altogether unexpected. The French physiologist Claude Bernard demonstrated that stimulation of the fourth ventricle of the brain caused glucose to rise, and it was later found that opiates put into this region of the brain could do the same thing.
This study reinforced the close links between metabolism and the brain, and gives us another reason for recommending that as we get older we must ensure that out glucose remains stable and that we do not become depressed.
Insulin Resistance in the Brain and What It Means for Dieters
Most people have been taught that increasing weight is the cause of insulin resistance, which in turn may cause an array of different health problems. That is only half true: insulin resistance may contribute to the development of obesity, and once we start gaining abdominal fat then that may indeed contribute to insulin resistance. So a vicious circle is established in which insulin resistance helps cause obesity, which in turn causes more insulin resistance.
Another thing that we have been taught for half a century that the brain is an insulin-insensitive tissue. What that means is that the uptake and use of glucose by the brain is not affected by circulating levels of glucose and insulin. That has always seemed a bit strange, because insulin is very important in cognition. Some experts believe that disturbances of insulin and closely related hormone – insulin like growth factor 1 (IGF-1) are involved in the pathogenesis of Alzheimer’s disease.
When someone is insulin resistant, they have high circulating levels of insulin, and an obvious question is whether these high insulin levels may interfere with the normal functions of the brain. This is not a new idea. It has been known for many years that high levels of triglycerides, that may be a marker for insulin resistance, may be associated with cognitive impairment in people with type 2 diabetes.
Now colleagues in London have found that people who have peripheral insulin resistance also have brain insulin resistance especially in two brain regions – the ventral striatum and prefrontal cortex – that are involved in appetite and reward.

It looks as if one of the reasons why people with insulin resistance become obese is that the normal link between the control of food intake and energy balance is broken.
This is yet more evidence that a simple diet will not work in the long term. If the problem is metabolic and involves damage to the mechanisms that control eating, the only way to help is to use a combined approach that deals not only with the composition of the diet, but the precise time when people should eat, and the psychological and social barriers that are left over from millions of years of evolution. I outline a comprehensive and highly successful weight management technique in Healing, Meaning and Purpose. Over the last few months I have had an enormous number of requests to expand that material into another book, and in between writing this blog, I am hard at work on completing a full account of exactly what we do to help people manage their weight.
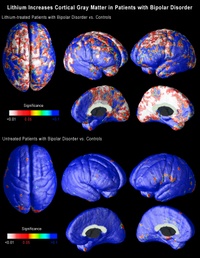
Lithium and Brain Growth
There’s an interesting story about the way that lithium was found to be helpful to some people with bipolar disorder. It was thought that there was a link between bipolar disorder and gout, and gout is caused by an accumulation of uric acid in some joints. It just so happens that lithium is very good at getting guinea pigs to pass any excess uric acid in their urine. So in 1949 a medical scientist in Australia called John Cade tried lithium in bipolar disorder. It worked, but not because of any effect on uric acid: the lithium/uric acid connection only works in guinea pigs. But now, all these years later, it turns out that there may actually be a link between bipolar disorder and uric acid after all: uric acid levels often rise in people who are insulin resistant, and insulin resistance is a common feature of bipolar disorder.
The last few years have seen the growth of an impressive body of evidence about the effects of lithium on the brain. Lithium modulates the way in which many neurotransmitters act in the brain. That raised interesting questions, because many of the chemical transmitters do not only send messages between neurons, they may also stimulate the growth of cell processes and perhaps neurons themselves. Then it was discovered that lithium protects neurons by increasing the levels of a neuroprotective protein called Bcl-2. Then it was found to help stimulate the production of new neurons (neurogenesis) in the hippocampus.
A major breakthrough came in 2000, with the demonstration that lithium increases the amount of gray matter in the human brain, probably by stimulating the production of a growth promoter called brain-derived neurotrophic factor. Gray matter is composed primarily of neurons, so this suggested that lithium was either stimulating the growth of new neurons, or causing the migration of neural stem cells, or alternatively somehow preventing the death of neurons.
Within less than two years it was confirmed that treatment with lithium increased the amount of gray matter in the brains of people with bipolar disorder.
The findings remained controversial for two reasons: first was the seeming impossibility of stimulating the production of new gray matter. That is no longer such a problem: there is more and more evidence that the adult brain can indeed produce new neurons.
The second problem was technology: the measurements were open to
different interpretations.
Now neuroscientists at UCLA, using brain scans collected by collaborators at the University of Pittsburgh School of Medicine have shown that lithium does indeed increase the amount of gray matter in the brains of patients with bipolar disorder. But what is far more important is that the effects are seen in precise regions of the brain that are thought to be implicated in bipolar disorder.
The research is published in the July issue of the journal Biological Psychiatry.
Carrie Bearden, a clinical neuropsychologist and assistant professor of psychiatry at UCLA, and Paul Thompson, who is associate professor of neurology at the UCLA Laboratory of NeuroImaging, used a novel method of three-dimensional magnetic resonance imaging (MRI) to map the entire surface of the brain in people diagnosed with bipolar disorder. Everyone interested in the brain has been amazed by the quality of the images coming from the UCLA lab over the last six or seven years. (Graphics from the study, including the one above, are available online here.)
When the researchers compared the brains of bipolar patients on lithium with those of people without the disorder and those of bipolar patients not on lithium, they found that the volume of gray matter in the brains of those on lithium was as much as 15 percent higher in the cingulate and paralimbic regions of the brain, that are critical for attention, motivation and emotional control. There was no change in the amount of white matter, telling us that these effects are unlikely to be either artifacts or swelling of the brain.
These are extraordinary findings that may help explain how lithium works. If lithium increases the amount of gray matter in specific regions of the brain, this may suggest that existing gray matter in these regions may be underused or dysfunctional in people with bipolar disorder.
Conventional MRI studies in bipolar disorder measured the total volume of the brain, but these new imaging techniques employ high-resolution MRI and cortical pattern-matching methods to map gray matter differences that are so precise that they can pick up subtle differences in brain structure and this is the first time that researchers have been able to look at specific regions of the brain in people with bipolar disorder, and examine the effects of treatment.
The researchers at UCLA analyzed MRI scans of 28 adults with bipolar disorder, 20 of whom were lithium-treated, and 28 healthy control subjects collected by collaborators at the University of Pittsburgh. The analysis involved detailed spatial analyses of the distribution of gray matter by measuring local volumes of gray matter at thousands of locations in the brain.
This is superb research, and one of the signs of good research is that it raises yet more questions:
- We do not know whether these effects on gray matter persist once the medicine is stopped.
- Neither do we know whether the same effect might occur in other illnesses in which there is loss of gray matter. It may just be that lithium corrects an abnormality that is specific to bipolar disorder. That being said, there is recent evidence that lithium may be neuroprotective in a mouse model of Alzheimer’s disease.
- We also do not know if these brain changes correlate with clinical improvement.
- Lithium can have a lot of side effects, so we shall also need to factor that into the equation.
- We also need to know whether other medicines – or any other kind of therapy – might produce similar effects: there are already several medicines that have been shown to do something similar in some animals.
It’s still a bit too early to suggest putting lithium in the water supply…
Dying of a Broken Heart
Some colleagues in London have discovered how intense stress may cause severe irregularities (arrhythmias) of the heart that could be fatal.
It has been known for some time that emotional trauma and psychological stress can precipitate cardiac arrhythmia and sudden death through over-activity of the sympathetic nervous system, the system usually associated with “Fight or flight.” It has also been known that people with preexisting heart disease are particularly at risk. This is one stereotype that is true: if someone with heart disease gets a bad shock, they may indeed die. It has been known for centuries that suffering a sudden unexpected bereavement can be a fatal stressor.
It is extremely important to understand how stress can affect the heart, and researchers at the Wellcome Trust Centre for Neuroimaging at University College London and the Brighton and Sussex Medical School have made an important breakthrough that has just been published in the Proceedings of the National Academy of Sciences. Measuring the electrical activity of the brain and heart at the same time, they discovered at the regions of the brain responsible for learning, memory and emotion can destabilise the cardiac muscle of someone who already has heart disease. These areas of the brain can participate in a “vicious cycle” with the heart.
The patients performed the task of counting backwards in sevens, which is for most people mildly stressful.
The researchers discovered that activity in “higher level” regions of the brain such as the cerebral cortex, not only reflected the responses of the heart to stress, but also became involved in a “feedback loop”, often worsening the situation by making the heart muscle less stable.
The regions of the brain responsible for regulating heart function can be unbalanced by stress, and it can be fatal.
It is further evidence that there is a constant “conversation” between the heart and the brain.
It is also the best evidence to date that comprehensive care of people with heart disease must include stress management.
And why wait until it’s too late?
Now is the time to start building your resilience to stress!
Stem Cell Treatment for Cerebral Palsy?
Medical News Today is carrying a interesting article entitled, “Dramatic Improvement For 19-Year-Old Hungarian Cerebral Palsy Sufferer After Stem Cell Treatment.”
According to the report a 19-year-old from Hungary named Gabor Bocskai had stem cells injected into the fluid around his spinal cord.
It goes on to say,
“The successful procedure, performed at China’s top stem cell facility, makes Mr. Bocskai the first teenage European CP patient to
see rapid improvement through stem cell therapy. Unedited
videos taken before and after Mr. Bocskai’s injections dramatically demonstrate the profound improvement in his 19-year battle to walk, write, focus his eyes, concentrate, and overcome the many other detrimental effects resulting from the CP he acquired at birth. More details and the videos have been published on China’s leading Stem Cell News site at http://www.stemcellschina.com.
Some of Mr. Bocskai’s most noticeable and immediate physical
improvements after the eight-week stem cell therapy program
include improved vision, increased eye focus and better
concentration on one subject. He also reported clearer writing, enhanced muscle tone, the ability to sit up unsupported, and a new capability to walk and swim in an unassisted manner. As a lifelong quadriplegic with paralysis in his lower limbs, Mr. Bocskai was never able to walk independently, using a wheelchair for transportation. Within four months of the initial treatment, he stated that he was able to walk with the help of a walker and no other support, and at a rate three times faster than ever before with increased maneuverability in his legs and torso. Even his
speech became clearer and faster.
In Mr. Bocskai’s most recent blog entry dated March 11, 2007, he excitedly stated, “My ability to concentrate has increased up to 6 hours a day as a result of stem cell treatment, so studying is much easer than before. I no longer get tired from learning.” (Gabor’s CP Blog is at
http://www.stemcellschina.com/blogs/Gabor%20cp/)The
Hospital announced that Mr. Bocskai has since returned to
Hungary from China and has reported continued daily
improvement. It also cautioned that not every teenage CP
patient treated with stem cell therapy should expect the
same impressive results.”
There is very little information on the procedure, and I could not find any information about where the stem cells came from. I do see that he also had “certain medications” as well as hyperbaric oxygen.
The article is so enthusiastic that it reads like an advertisement!
I do very much hope that Gabor gets some real help from all of these treatments, but we need to be very cautious until we have a great deal more information not just about the science, but also the ethics of the treatment that he has had. For example, where did the stem cells come from? Do we know that they were stem cells?
It is always great to hear about success stories, but sad to say, we then need to do the boring bit: the checking, the testing and the replicating that go into sustainable medical progress.
I have done an extensive literature search and cannot find any published scientific reports, but I only covered the languages that I can read. So there could be something in Chinese that I missed.
I shall let you know immediately if we find out any more about the use of stem cell treatments in humans.






