Mature Plasticity in the Human Brain

The more we look, the more we understand that the human brain retains a remarkable ability to learn and re-fashion itself well into old age. The old idea that young brains are flexible, but that age causes us to become “hard-wired” and inflexible is not correct.
This has been confirmed in some new research that has just been published in the journal Neuron by investigators from Johns Hopkins who have shown that adult neurons are not glued in place as rigidly as had been thought.
The investigators led by David Linden used a new technique known as two-photon microscopy that allowed them to living neurons at work in the intact brain. The researchers injected fluorescent dye into the brains of mice to illuminate a subset of neurons and then viewed these neurons through a window in the skull of living, anesthetized mice.
They examined neurons that extend axons to the cerebellum, a region of the brain involved in coordinating motor and sensory information. These axons have a primary trunk that runs upward and several smaller branches that sprout out to the sides.
While the main trunk was firmly connected to other target neurons in the cerebellum, the side branches were mobile: Linden describes them like this:
“The side branches swayed like kite tails in the wind.”
Over the course of a few hours, individual side branches would highly dynamic behavior, elongating, retracting and morphing. These side branches also failed to make conventional synaptic connections with adjacent neurons. The motion of the side branches was arrested stalled by a drug that produced strong electrical currents in the axons.
Why the brain would want such motile, non-connected branches remains a mystery.
They may provide a second mechanism for conveying information beyond traditional synapses. Alternatively they may be involved in nerve regeneration.
Whatever the final answer, it is clear that the adult brain remains a remarkably plastic, fluid and flexible structure.
Excellent news for all of us!
“That which is flexible and flowing will prosper and grow. That which is rigid and blocked will wither and die.”
–Tao te Ching
“When a noble life has prepared old age, it is not decay that it reveals, but the first days of immortality.”
–Muriel Spark (Scottish Writer, 1918-)
“You will stay young as long as you learn, form new habits and don’t mind being contradicted.”
–Marie, Baronin von Ebner-Eschenbach (a.k.a. Baroness Marie von Ebner-Eschenbach, Austrian Writer, 1830-1916)
Attention Deficit Disorder and the Growing Brain
An extremely important article by researchers from the National Institute of Mental Health has just been published in the Proceedings of the National Academies of Sciences. It suggests that children with Attention Deficit Hyperactivity Disorder (ADHD) have brains that develop more slowly than those of children without ADHD. However in most cases they still follow a normal pattern of development.
In a study of 450 children, 225 of whom had ADHD, the researchers found that the cerebral cortex of children with ADHD developed about three years more slowly.
The primary measure that they used was the peak thickness of the brain, which is normally taken to be a sign of maturity. Half of the children with ADHD reached peak thickness when they were an average of 10.5 years old, compared with 7.5 years among children without ADHD.
Even if the brain is developing more slowly, the fact that it appears to grow normally is reassuring, and may explain why a substantial proportion of children with ADHD do grow out of it as they get older. Though it still leaves us with several questions:
- Why does the delay occur at all?
- Why do so many people NOT grow out of it, and have persistent symptoms in adulthood?
- Is the brain really “catching up?” The brains of people without ADHD also continue to develop and grow
The National Institute of Mental Health has also published a nice press release that includes a video of brain maturation. You can find it here.
Close Your Eyes and I’ll…

Every young neuroscience student learns about a classic experiment that was published in 1956 by Raul Hernandez-Peon, in which he had an electrode in the acoustic nerve of a cat, while a metronome was ticking. Every tick caused a pulse of electricity in the nerve. But as soon as the cat saw or smelled a mouse, the electrical activity plummeted: now all of his attention was on lunch, and his brain damped down the unnecessary ticking of the metronome. Something similar happens with the “Cocktail Party Phenomenon:” our ability to focus our listening attention on a single talker and ignoring other conversations that are going on.
A study by researchers from Wake Forest University Baptist Medical Center and the University of North Carolina was presented at the Society for Neuroscience conference in San Diego this week, suggesting that our brains can turn down our ability to see, so that we are better able to listen and focus on music and complex sounds.
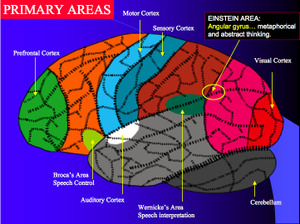
The research used functional Magnetic Resonance Imaging in 20 non-musicians and 20 musical conductors aged 28-40, and found that both groups diverted brain activity away from visual areas during listening tasks. The activity fell in the visual regions areas as it rose in auditory ones. But during harder tasks the changes were less marked for conductors than for non-musicians.
While being scanned the subjects were asked to listen to two different musical tones played a few thousandths of a second apart and identify which was played first. The task was made harder for the professional musicians than for the non-musicians, to allow for the differences in their background.
As the task was made progressively more difficult, the non-musicians carried on diverting more and more activity away from the visual parts of the brain to the auditory, as they struggled to concentrate on the music. However, the conductors did not suppress their brains, suggesting that their years of training had given them an advantage in the way that their brains were organized and functioning. They are less likely to be distracted and are highly tuned to musical sounds.
This is like closing your eyes to listen to music and the advantage of the trained musicians is similar to the advantage that we see in the brain of the chess master compared with the amateur. Years of study and practice enable the chess player to move without much conscious thought.
It shows how well we are able to divert activity from one part of the brain to another as needed. It is that ability to be flexible and to recruit more brain when we need it that lies at the heart of the neurocognitive revolution that is changing the way that we think about the brain and mind.
Minocycline and Neurological Disease

We recently talked about the fascinating new data on the use of the antibiotic minocycline for treating stroke. The reason is that minocycline is also an anti-inflammatory and it also prevents “apoptosis” or programmed cell death. It has been found to be neuroprotective in animal models of stroke, traumatic brain injury and neurodegenerative disorders. Minocycline also prolongs survival and reduces the loss of motor neurons in transgenic mouse models of amyotrophic lateral sclerosis (ALS), a.k.a. motor neuron disease, a.k.a. Lou Gehrig’s disease.
But as with any new research, we always have to go back and re-check and replicate everything. How many times have you heard a news item about some major breakthrough, and then you never again hear anything about it?
An article in today’s issue of the Lancet has indicated that minocycline may be harmful to people with ALS. This is important and will have implications for several clinical trials that are either planned or in progress for trying minocycline in people with dementia, stroke, Huntington’s disease and multiple sclerosis.
The United States Western ALS Study Group based at Columbia University in New York, undertook a randomized phase III trial to test the efficacy of minocycline as a treatment for ALS in 412 patients. Patients who took minocycline deteriorated at a 25% faster rate compared with people on placebo.
Therefore the authors suggest that trials of minocycline in other neurological diseases should be reassessed. It is possible that minocycline might be detrimental in patients with other neurological diseases as well.
There is also an editorial comment by Mike Swash, who was once one of my teachers. He talks about the importance of early diagnosis in ALS:
“Clinicians and patients alike would prefer ALS therapy to be tested as early as possible, but there are unresolved difficulties with accurate early diagnosis, particularly the absence of a specific diagnostic test. Might some of the compounds that have failed in clinical trials show benefit if tested at disease onset in human beings?” He concludes that the time has come for new approaches to trial design: “The aim must be to design informative, short, inexpensive, and sensitive phase I/II studies before large phase III studies are attempted”.
This is another one of those examples where a medicine introduced for one indication may have many others. In contrast to an antibiotic being used to treat neurological problems, there has recently also been a great deal of interest in the antibiotic potential of some medicines used to treat depression and psychosis.
There is a mountain of new information on this topic, which promises to revolutionize many of our concepts of health and disease. I shall keep you posted as more material is published.
Rewiring the Dyslexic Brain

Dyslexia can be a real difficulty for many children, although for many it has been a gift: they have succeeded very well in life by mobilizing other psychological and neurological resources. Sir Richard Branson, the founder of Virgin Enterprises, Thomas Edison and Albert Einstein are all said to have had dyslexia.
There are many types of dyslexia, but in the most common – developmental dyslexia – children confuse letters and syllables when they read.
It now appears that some children with dyslexia struggle to read because their brains are not correctly wired to process fast-changing sounds, according to a study published this month in the journal Restorative Neurology and Neuroscience.
However sound training using computer exercises was able to rewire children’s brains, correcting the sound processing problem and improving reading.
More than 30 years ago Paula Tallal of Rutgers University proposed that children with dyslexia might have an underlying problem processing sound, but it has never been tested using brain imaging. The researchers used functional MRI imaging (fMRI) to examine how the brains of twenty two 9- to 12-year old children with developmental dyslexia, and normal readers, responded to sounds, both before and after using educational software called Fast ForWord Language.
The first test involved measuring how the children’s brains responded to either fast-changing or slow-changing sounds that resembled speech. The fast-changing sounds altered in pitch or other acoustic qualities quickly. In just tens of milliseconds, as occurs in normal speech. The slow-changing sounds changed over only hundreds of milliseconds.
In normal readers, 11 brain areas became more active when the children listened to fast changing, compared to slow changing, sounds. In dyslexic children, the fast-changing sounds did not stimulate high levels of activity in these regions of the brain. Instead, dyslexic children processed the fast-changing sounds as if they were slow changing. They used the same regions of the brain but at lower intensity.
We know that infants must correctly process fast-changing sounds as they learn language. They use sound processing to create a sound map of their native language. If they are unable to analyze fast-changing sounds, their sound map may become confused. The idea is that they run into trouble when they first see printed letters because the children’s brains now try to match their internal sound map to letters that they see on the page. Linking normal letters to confused sounds may lead to syllable-confused reading.
But the brains of the children with dyslexia changed after completing exercises in a computer program known as
The Fast ForWord Language program does not involve reading at all, but only listening to sounds, starting with simple, changing noises, like chirps that swooped up in pitch. The children then have to respond with a clicker when the chirp’s pitch goes up or down. At first the sounds are played slowly, but they gradually speed up, becoming more challenging for dyslexic children. The exercises are then repeated with increasingly complex sounds: syllables, words, and finally, sentences.
The fMRI study showed that these repetitive exercises appeared to rewire the dyslexic children’s brains: after eight weeks of daily sessions – about 60 hours in total – their brains responded more like the brains of typical readers when they were processing fast-changing sounds, and at the same time their reading improved.
It is still early days for this research, and we do not yet know whether the improvements in reading and in the brain will be sustained.
This research may make it possible to identify children at risk of dyslexia even before they start learning to read. It is also possible that other approaches to learning sounds, such as learning to sing or play an instrument may be effective, since most of us learn music with gradual, repetitive, and intense listening and move up to faster changing sounds.
Decision Making and Internal Balance

Many of us run into problems when we try to make decisions. In a special section in the October 26 issue of the journal Science, Martin Paulus who is a professor in the Department of Psychiatry at the University of California in San Diego, has marshaled a growing body of evidence that human decision-making is inextricably linked to an individuals’ need to maintain a homeostatic balance.
He goes on to suggest that psychiatrists may need to approach the treatment of psychiatric patients from a new direction: by understanding that such individuals’ behavior and decision-making are based on an attempt to reach an inner equilibrium, in the same way that we try to being our temperature or blood pressure back to a set point. And if the thermostat is broken we may see mental illness and substance abuse.
This makes good sense: in the past decision-making process as a considered series of options and values, but that is not what we see in the clinic. People with addictions and some mental illnesses keep making bad choices, despite being intelligent and insightful.
Recent neuroimaging research shows strong support for the homeostatic nature of decision-making:
The insula is involved in processing interoceptive information: the body’s internal state or sense of balance
Damage to the insula stops addiction to cigarettes
Some of the same brain structures implicated in the urge to take drugs are involved in other biological urges
The question addressed in part by this paper are whether changes in decision-making behavior and associated brain functions are a result of pre-existing characteristics – which may predispose individuals to use drugs – or occur as a consequence of long-term use.
This is certainly an interesting idea, and we shall have to see how it fits as we collect further data.
“The quality of a decision is like the well-timed swoop of a falcon which enables it to strike and destroy its victim.”
–Sun Tzu (Chinese Military Strategist and Author of the “Art of War”, c.400-c.430 B.C.E.)
“The risk of a wrong decision is preferable to the terror of indecision.”
–Maimonides (a.k.a. Rabbi Moses ben Maimon, Spanish-born Jewish Philosopher and Physician, 1135-1204)
“All you have to decide is what to do with the time that is given you.”
–J.R.R. Tolkien (South African-born English Writer, Linguist, Oxford Don and a Member of C.S. Lewis’ Literary Group, “The Inklings,” 1892-1973)
“Decisions are doorway to change and change starts from a moment of decision. One decision can change your life forever!”
–Tony Robbins (American Motivational Speaker and Writer, 1960-)
“Nothing is more difficult, and therefore more precious, than to be able to decide.”
–Napoleon Bonaparte (Corsican-born French Military Strategist, General and, from 1804-1814, Emperor of the French, 1769-1821)
Optimism and the Brain

Humans have a wonderful ability to expect positive events in the future, even when there is no shred of evidence to support them. One of the key components of resilience is optimism. Though there is data to show that there is a genetic contribution to optimism, it is also a psychological attribute that can flow from life experiences as well as attitude that can be developed. Though the motivational coaches who tell us that putting on a happy face will make you happy and optimistic are probably overstating the truth! A lack of optimism is often a sign of clinical depression so learning more about it, is not just an academic exercise.
New research just published in the journal Nature indicates that there are two regions of the brain linked to optimism.
The team from New York University and University College, London, says that the act of imagining a positive future event, for example winning an award or receiving a large sum of money, activates two brain areas: the amygdala and the rostral anterior cingulated cortex (rACC). The finding ties in with earlier studies that suggested that these brain regions malfunction in depression. (1,2)
The investigators first measured how optimistic 15 volunteers were using a standard questionnaire. They were then scanned using functional magnetic resonance imaging (fMRI) while reflecting on one of a number of potential scenarios.
In one part of the trial, subjects followed specific instructions to recall a negative event in the past, such a funeral that they had attended in the past five years. In another experiment they had to imagine what it would be like to be involved in a car crash in the near future. At other points in the study subjects had to reflect on positive events such as winning an award in the past or receiving a large sum of money in the future.
Reflecting on both past and future events activated the amygdala and the rACC regions of the brain. However, positive events, and particularly those imagined in the future, generated a significantly larger response in these regions than reflecting on negative events.
When imagining happy events, the more pessimistic subjects in the trial had less activation of these brain areas than their optimistic counterparts when imagining happy events.
For some time now, many researchers have assumed that the amygdala and rACC are only involved in negative thoughts and negative reactions, but this research indicates that they have an important role in signaling cheerful thoughts. And, what is more, these are also regions of the brain that have been implicated in depression. Previous research has suggested that patients with depression have decreased nerve signaling and fewer cells in the rACC and amygdala.
Is this why people with depression find it so hard to generate positive thoughts?
This is important work that will likely have a great many practical applications.
“Children are born optimists and we slowly educate them out of their heresy.”
–Louise Imogen Guiney (American-born English Poet, 1861-1920)
“Although the world is full of suffering, it is full also of the overcoming of it.”
–Helen Keller (American Blind and Deaf Swedenborgian Philosopher, 1880-1968)
“No man is so old as not to think he can live one year more.”
–Marcus Tullius Cicero (Roman Political Figure and Orator, c.106-43 B.C.E.)
“The way to become happy
Is to think
And to feel
That the very best is yet to come.”
–Sri Chinmoy (a.k.a. Chinmoy Kumar Ghose, Indian Philosopher and Spiritual Teacher, 1931-2007)
The Neurology of Fibromyalgia

Fibromyalgia can be a particularly nasty illness, not least because people who suffer from it have often been misdiagnosed and occasionally even accused of malingering. But the pain can be very real and very severe. There are some very good reasons for believing that it is a neurological problem involving regions of the brain and spinal cord that are involved in modulating pain.
A new study from the University of Bath and Royal National Hospital for Rheumatic Diseases in England has raised some intriguing possibilities for treatment. A year ago, researchers from the same institution reported that there is a reorganization of the sensory regions of the brain n people with chronic pain.
In this new study, researchers asked patients to look at a reflection of one arm while moving their other arm in a different direction that was hidden behind a mirror positioned in front of them at a right angle. So one limb was obscured from view behind the mirror while they could clearly see the other limb and its reflection.
This simple experiment created a mismatch between what the brain sees from sensory input and what it feels through the motor system that controls movement.
Of the 29 fibromyalgia patients involved in the study, 26 reported feeling a transient increase in pain, temperature change or heaviness in their hidden limb – all symptoms of a flare up of their condition.
This suggests that a mismatch between sensory and motor neurons could be at the root of the fibromyalgia.
This study adds to the growing body of evidence that many of the symptoms of fibromyalgia may be triggered or perpetuated by a sensory-motor conflict.
That opens up all kinds of new possibilities for treatment.
Sleep Deprivation and Emotional Instability

Most of the time we are in control of our moods, rather than our moods being in control of us. One of the main things that we learn as we get older is not simply to damp down our emotional reactions, but to make them “contextually relevant:” we produce the right emotional response for the right situation. Yet we also know that there are exceptions: times when our emotions over-run any attempts at our control.
Second, we all know that sleep deprivation can be a Bad Thing. It is known to impair a range of mental and physical activities, including immune function, metabolic control and many cognitive processes, including learning and memory.
It has long been suspected that sleep deprivation can have significant effect on mood. Many of us feel irritable and distractible if we haven’t slept enough, and you may have had the experience of being up all night and feeling a little bit “high” in the morning. It has also been known for centuries that mood disorders are very commonly associated with sleep disturbances, and sleep disturbance is often the first sign that someone with mood problems is running into trouble. So mood and sleep must be linked in some way.
Despite these common observations, there has never been that much empirical evidence for the impact of sleep deprivation on mood, and in particular the effects of sleep deprivation on the brain.
An important new study by researchers from Harvard Medical School and the University of California at Berkeley has just been published in the journal Current Biology, and it is beginning to fill in some of the gaps in our knowledge.
The amygdala is known to be involved in processing of emotionally salient information, particularly unpleasant or aversive stimuli. In mature individuals, the emotional centers of the brain are usually controlled and modulated by an array of connected systems, mainly in the frontal regions of the brain. One particularly important part of the frontal lobes that is involved in controlling the amygdala is the medial-prefrontal cortex (MPFC). Under normal conditions the MPFC is supposed to exert an inhibitory, top-down control of the amygdala, so that we only generate appropriate emotional responses.
The scientists worked with 35 volunteers who were deprived of sleep for 35 hours. Blood flow can be used to deduce which specific regions of the brain are active. The researchers used functional magnetic resonance imaging (fMRI) to examine the blood flow – and therefore activity – in the brains of the volunteers in real time, both during and after sleep deprivation.
After going without sleep, the participants were asked to look at images that were designed to trigger angry or sad emotional responses. The investigators discovered that the amygdala showed 60% higher reactions to the images compared with people who are not sleep-deprived.
This is an extraordinarily large effect and implies that sleep deprivation knocks out the normal control mechanisms in the frontal lobes so that the sleep-deprived brain reverts to a more primitive pattern of activity. As a result we become unable to put emotional experiences into context and produce controlled, appropriate responses.
If we needed any more reasons to get a good night’s sleep, this one is very powerful. It also re-iterates something very important: if you or a loved one have had problems with mood, anger or anxiety, it is essential to watch your sleep pattern. Any change may be a harbinger or trouble, and is an excellent early warning that you or they need a hand to make sure that things stay on an even keel.
“Your brain shall be your servant instead of your master, you will rule it instead of allowing it to rule you.”
–Charles E. Popplestone (American Author of Every Man a Winner, 1936)
“Control your emotions or they will control you”
–Chinese Proverb
“For the uncontrolled there is no wisdom, nor for the uncontrolled is there the power of concentration; and for him without concentration there is no peace. And for the unpeaceful, how can there be happiness?”
–Bhagavad Gita (Ancient and Sacred Sanskrit Poem Incorporated into the Mahabharata)
“He who controls others may be powerful, but he who has mastered himself is mightier still.”
–Lao Tzu (Obscure Chinese Philosopher, Founder of Taoism and Alleged Author of the Tao-Te Ching, c. 604-c. 531 B.C.E.)
“ . . . let every man be swift to hear, slow to speak, slow to wrath.”
–The Bible, James 1:19
“When angry, count ten before you speak; if very angry, a hundred.”
–Thomas Jefferson (American Writer, Philosopher, Politician and, from 1801-1809, 3rd President of the United States, 1743-1826)
Dopamine, Drugs and Diabetes
We recently talked about the increasing evidence that insulin has many extremely important roles in the brain.
New research by investigators at the Center for Molecular Neuroscience and the Institute of Imaging Science at Vanderbilt University Medical Center researchers, working with colleagues in Texas, has found that insulin levels affect the brain’s dopamine systems. These systems are involved in motivation, reward, salience, movement and emotional processing. Disturbances in dopamine pathways have been implicated in substance abuse, as well as schizophrenia, bipolar disorder and attention deficit hyperactivity disorder (ADHD). Drugs that interfere with the dopamine pathways may produce Parkinsonism as well as elevations of the hormone prolactin.
The psychostimulant drugs amphetamine and cocaine, as well as related medications for ADHD, block the reuptake of the neurotransmitter dopamine by dopamine transporters (DATs) thereby increasing the level of dopamine signaling. Some of these compounds also cause a massive surge of dopamine through DATs, resulting in high levels of synaptic dopamine that alter attention, increases motor activity and plays an important role in the addictive properties of psychostimulants.
The reason for examining a possible relationship between dopamine and insulin goes back to the 1970s, when it was reported that amphetamine had no effect on diabetic animals and in the 1980s it was shown that diabetic rats did not show the usual stereotyped behaviors when given amphetamine. There were also odd reports about disturbances in the enzyme dopamine-beta-hydroxylase in experimental diabetes and changes in dopamine D1 receptors in the brains of rats with induced diabetes.
These observations lead to this new research into a possible link between insulin signaling and amphetamine action.
They used a standard a rat model of type 1 diabetes in which insulin levels are massively depleted, and then assessed the function of the dopaminergic pathway in the striatum, an area of the brain rich in dopamine.
In the absence of insulin, amphetamine-induced dopamine signaling was disrupted: dopamine release in the striatum was severely impaired and expression of DAT on the surface of the nerve terminal was significantly reduced.
The lack of the DAT protein on the plasma membrane prevents the amphetamine-induced increase in extracellular dopamine, and in turn, amphetamine fails to activate the dopamine pathways that stimulate reward, attention and movement.
The researchers then gave insulin into the brains of the diabetic animals and found that the system returns to normal, indicating that the lack of insulin in the striatum directly affected amphetamine action.
They also developed a probe for brain DAT activity using functional magnetic resonance imaging (fMRI). In normal, healthy rats with plenty of insulin, amphetamine increased neural activity in the striatum. But in diabetic animals, activity in the striatum was suppressed.
So there is a powerful interplay between dopamine neurotransmitter systems and insulin signaling mechanisms. The results are some of the first to link insulin levels and dopamine function in the brain and hold several implications for human health and disease.
We need to have another look at the effect of diabetes on the brain. We have known that people with diabetes are at increased risk of cognitive impairment and depression, and we had assumed that it was because of hypoglycemia and vascular disease. Those assumptions may have been wrong.
The findings may also be important for diseases with altered dopamine signaling, such as schizophrenia and ADHD. Insulin may have something to do with the underlying brain disturbances in ADHD. Then control of insulin levels and neuronal responses to the hormone may help determine the efficacy of psychostimulants in people with ADHD.
Every now and then you see people on psychostimulant medications who need huge doses. Perhaps their problem lies with insulin rather than dopamine.






