A New Treatment for Toxoplasmosis
I have talked at some length about the possible link between toxoplasmosis and some forms of mental illness, but there is also another side to toxoplasmosis: the Toxoplasma gondii parasite infects nearly one-third of all humans: more than two billion people worldwide. In the United States alone, congenital toxoplasmosis occurs in an estimated 1 per 5,000 births a year and can cause severe vision loss, brain damage and even death. The human cost is incalculable, and in dollars and cents, it has been estimated that the annual cost of caring for these children may exceed $1 billion.
Toxoplasma gondii is carried by some cats and it is said that an infected cat can excrete up to 20 million oocysts over a period of two weeks, and every single oocyst is infectious. They are tenacious and can remain infectious in water for up to six months and in warm moist soil for a year of more.
Toxoplasma infects humans through three main routes:
- Consumption of undercooked, infected meat
- Ingestion of T. gondii oocysts in food, through accidental contamination from cat litter
- Finally, a newly infected pregnant woman may pass the infection to her fetus, hence the warning that pregnant women should not clean the cat box
Not only is toxoplasmosis the most common parasitic infection in the world, but also it can cause particular problems in people with compromised immune systems, for instance people with cancer, autoimmune disease, AIDS or transplant recipients.
It is even possible for people with normal immune systems to suffer major organ damage from chronic infections. Eye disease leading to loss of sight can be caused both a primary infection and as a result of infection transmitted from mother to child. Damage to other organs has recently caused deaths among otherwise healthy young people during epidemics in Surinam and French Guiana.
The parasites that cause malaria are related to Toxoplasma gondii, and a new drug that will soon enter clinical trials for the treatment of malaria also appears to be 10 times more effective than the current gold-standard treatment of toxoplasmosis, a combination of the drugs pyrimethamine and sulfadiazine.
In the March issue of PLoS Neglected Tropical Diseases, a research team based at the University of Chicago Medical Center reports that the drug, known as JPC-2056, is extremely effective against Toxoplasma gondii, both in cell culture and in mice, and apparently without the toxicity associated with the current standard treatment.
The drug works inhibiting the action of the from of the enzyme dihydrofolate reductase (DHFR) that is produced by the family of parasites that includes those that cause toxoplasmosis and malaria, and in cell culture studies, the drug appears actually to kill the parasite, rather than simply preventing its replication. This is very important: not only do most of the current medications have a good many side effects, they have little effect on Toxoplasma during certain phases of its life cycle. It can hunker down in the quiescent cystic phase and wait until the antibiotics are gone.
Rima McLeod, professor of ophthalmology and specialist in infectious diseases at the University of Chicago said,
“JPC-2056 has the potential to replace the standard treatment of pyrimethamine and sulfadiazine. Taken by mouth, is easily absorbed, bioavailable, and relatively nontoxic. In tissue culture and in mice, it was rapidly effective, markedly reducing numbers of parasites within just a few days.”
JPC-2056 is not a new drug. It was developed in the late 1980s by teams led by Wilbur Milhous and Dennis Kyle of the Walter Reed Army Institute for Research and David Jacobus of Jacobus Pharmaceutical Company. The original version was quite toxic, but the researchers found ways to reduce the toxicity and developed an oral version of the drug. Clinical trials using JPC-2056 to treat malaria are scheduled to begin later this year.
Bobby Fischer R.I.P.
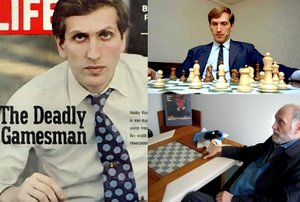
News services round the world have been reporting the untimely death of Bobby Fischer, a.k.a. Robert James Fischer, the American-born chess genius.
Fischer’s match with Boris Spassky in 1972 had a huge influence on me, tempting me back to competitive chess, and over the years I studied most of his games in great detail. So I was definitely a fan.
But sadly much of the coverage has focused on some of the foul things that he said in his later years. It is particularly unfortunate because most of the reports failed to mention a number of other things about him.
I never met or examined Fischer and it is dangerous to diagnose people at long range. But there were multiple reports that made it very clear that he long ago crossed the line into mental illness.
He was always single-minded and cantankerous, and some of his allegations about cheating turned out to be correct. But when he began to believe that people could pick up or manipulate his thoughts through the fillings in his teeth, it was clear that something else was going wrong with him.
Some people have tried to link genius in chess and mental illness, but the link is at best tenuous, even though more than one very strong player has succumbed to mental illness. As we have discussed, there may be a link between creativity and schizotypal personality disorder, but the thing about chess is that high-level play requires enormous sustained concentration and motivation, to say nothing of the ability to withstand intensive mental stress. Thos are all things that become difficult as mental illness progresses.
One of the best ways of evaluating a culture is the way in which it treats its weakest members. So let us remember and celebrate Fischer’s genius and recognize that his later and ever darker life was driven by a terrible mental deterioration.
“The chessboard is the world, the pieces are the phenomena of the Universe, the rules of the game are what we call the laws of Nature. The player on the other side is hidden from us.”
–Thomas Henry Huxley (English Biologist and Educator, 1825-1895)
“Chess is the touchstone of intellect.”
–Johann Wolfgang von Goethe (German Poet, Playwright and Philosopher, 1749-1832)
Schizophrenia and Evolution

Schizophrenia remains one of the cruelest illnesses ever to afflict humanity. There are more theories about it than any other problem, and we may be getting closer to understanding why it seems to occur only in humans, and at roughly the same rate throughout the world. One idea is that the genetic predisposition to schizophrenia might have evolved as a secondary consequence of selection for human cognitive traits. As humans have evolved so has the brain, and it has become more lateralized, so this might explain the association between schizophrenia and handedness.
Several genes with strong associations to schizophrenia have evolved rapidly during human evolution, according to new research in the Proceedings of the Royal Society B this week.
In support of the cognition/schizophrenia hypothesis, researchers Dr Steve Dorus from the University of Bath, who worked with Dr Bernard Crespi from Simon Fraser University in Canada and Dr Kyle Summers from East Carolina University in the United States found that these genes had been positively selected.
They analyzed the molecular evolution of the 76 genes that have the strongest genetic association with the disorder. They surveyed human polymorphisms for discrete changes in the human genome that vary between individuals, in order to try and track very recent selective events within specific human populations. They also compared genes between mammalian species to identify selection on primate lineages salient to the evolution of humans and the disorder.
Amongst the genes for which they found positive selection were three genes that have the best functional or reproducible associations with the disorder: disrupted in schizophrenia (DISC1), dystrobrevin-binding protein 1 (DTNBP1) and neuregulin 1 (NRG1).
The selective forces underlying adaptive evolution of these genes remain largely unknown, but these findings are consistent with the hypothesis that schizophrenia is a maladaptive by-product of adaptive changes during human evolution, perhaps associated with creativity and human cognition.
Mindfulness and Depression

Mindfulness meditation has rightly been receiving a lot of attention recently. It is quite simply a technique in which you become intentionally aware of your thoughts and actions in the present moment, non-judgmentally. Though originally a Buddhist technique, it is something that can be practiced by anyone, and there are, in fact, similar techniques that have been developed by Christian mystics and Sufis.
It has recently been discovered that some of the techniques that were developed so that a mystic or meditator could carry on without distraction, may also have value in treating clinical problems. After all, if a group of people has spent a thousand years developing tools and techniques for managing the mind, it might be a good idea to see what they have discovered!
There have recently been several excellent books on the use of mindfulness in the management of depression:
The Mindful Way Through Depression
Relaxation, Meditation and Mindfulness
Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition
This whole field was moved forward by some research from San Francisco (NR822) that was presented at the end of May at the 2007 Annual Meeting of the American Psychiatric Association in San Diego. The researchers used Mindfulness-Based Cognitive Therapy (MBCT) in a group of 53 people with treatment resistant depression.
MBCT is based on the Mindfulness-based Stress Reduction (MBSR) eight-week program that was developed by Jon Kabat-Zinn in 1979 at the University of Massachusetts Medical Center. Research has show that MBSR can be enormously empowering for people with chronic pain, hypertension, heart disease, cancer, and gastrointestinal disorders, as well as for psychological problems such as anxiety and panic.
Mindfulness-based Cognitive Therapy grew from this work. Zindel Segal, Mark Williams and John Teasdale adapted the MBSR program so that it could be used for people who had suffered repeated episodes of depression.
The results of the study presented in San Diego showed that MBCT was effective in reducing depression when compared to treatment as usual: what we call “TAU.” What seems to happen is that MBCT gives people a set of skills for detaching from the stream of depressive thoughts and feelings. As a result the symptoms decrease. Though the study will need to be expanded and replicated, this is clearly a fertile area for research.
This work is also interesting in the light of recent research showing that mindfulness training may improve the activity of some of the subsystems of the brain dedicated to attention, as well as helping some people with mental illness control their aggressive behavior. Mindfulness training may also help to reduce subjective reduces distress and improves positive mood states. It seems to be particularly good at reducing distracting and ruminative thoughts and behaviors.
And just for good measure, mindfulness may help some smokers quit.
“The purpose of meditation is not enlightenment, it is to pay attention even at extraordinary times, to be of the present, nothing-but-in-the-present, to bear this mindfulness of now into each event of ordinary life.”
–Peter Matthiessen (American Naturalist and Writer, 1927-)
“Meditation is not to escape from society, but to come
back to ourselves and see what is going on. Once there is
seeing, there must be acting. With mindfulness, we know
what to do and what not to do to help.”
— Thich Nhat Hanh Vietnamese Buddhist Monk, 1926-)
“Conscious means “having an awareness of one’s inner and outer worlds; mentally perceptive, awake, mindful.” So “conscious business” might mean, engaging in an occupation, work, or trade in a mindful, awake fashion. This implies, of course, that many people do not do so. In my experience, that is often the case. So I would definitely be in favor of conscious business; or conscious anything, for that matter.”
–Ken Wilber (American Philosopher, 1949-)
Musical Hallucinations

A paper on auditory hallucinations of music was presented
this afternoon at the 2007 Annual Meeting of the American Psychiatric
Association in San Diego, California.
The researcher looked at 22 people diagnosed with schizophrenia and
23 with schizoaffective disorder at Maimonides Medical Center in
Brooklyn, New York. The question was whether it would be possible to
use the presence of musical hallucinations to distinguish between
schizophrenia and schizoaffective disorder. The conclusions from the
study were that these auditory hallucinations of music were more common
in people with schizoaffective disorder and that voices with a
religious or superstitious content were more common in people with
schizophrenia.
Though it is good to see someone examine the content of hallucinations, this was a very puzzling study.
First, there is always a lot of debate around the “schizoaffective”
diagnosis. Although there are clear criteria for it in the DSM-IV, many
experts believe that most people who have been labeled
“schizoaffective” actually have a form of bipolar disorder. But in any
case, bipolar disorder and schizophrenia probably lie on a spectrum.
People’s diagnoses often change over time. Not because of disagreement
or inaccuracy, but because people change over time. The term
“phenomenological drift” has been used to describe this observation.
What that means is that we always need to be sure of the diagnosis at
the time of the study, rather than what was written in the chart in the dim and distant past.
The other point is that genuine musical hallucinations are very
rare. The world literature contains under a hundred papers in European
languages, and the classic paper,
published by German Berrios in 1991 was an analysis of just 46 cases.
Berrios is regarded by many as one of the finest phenomenologists in
Europe, so it is surprising that the investigator in New York found so
many cases.
It will be good to see if the author or someone else can replicate
the work. The classic teaching about musical hallucinations has been
that they:
- Are more common in women
- Are more common in people who have hearing problems or are deaf
- Are more likely to occur in people with neurological diseases, including Alzheimer’s disease
- If they occur in people with neurological disease, it is more
likely that the damage will be in the right or non-dominant hemisphere
of the brain. (In men, language tends to be in the dominant hemispheres
and music in the non-dominant. The pattern is a bit more complicated in
women, but they also usually sing and recognize music with the right or
non-dominant hemisphere)
A recent report from Japan reported that an elderly man with musical hallucinations was helped with the cholinesterase inhibitor donepezil (Aricept), suggesting that cholinergic neurons are somehow involved in generating musical hallucinations.
Many of us have music or tunes giong round in our heads, but that is quite different from hallucinating music.
And let me repeat: hearing things is common, and does not mean that someone is mentally ill.
House Supporting NAMI
Regular readers will know two things about me:
- I am a huge advocate for the mentally ill
- Last year I had to publish two denials after some mendacious individual posted the preposterous suggestion that the character of Gregory House in the wonderful TV show, was in some way based on me. To this day I don’t know where that idea came from, other than the fact that I have specialized in trying to crack diagnostic conundrums.
Take the two together, and I’d like to give credit where it’s due.
I was delighted to see that the entire cast and crew got together to support the National Alliance of the Mentally Ill (NAMI).
House has a well known expression, "Everyone lies." The the show’s producers and cast members, along with the slogan, will benefit the organization and its work in education, support, and advocacy for individuals and families affected by mental illness.
For a limited time, T-shirts from the show, emblazoned with the phrase "Everybody Lies," are being sold on-line.
The executive producer of house is Katie Jacobs, and she had this to say:
"Mental illness is stigmatized and misunderstood in our society, and we’re trying to do something about that. We’re very fortunate to be celebrating an extremely successful third season for HOUSE, and we’d like to give something back to a cause we feel is both worthy and overlooked."
The TV show, in the course of showing Dr. House attempting to diagnose illnesses with hallucinatory or psychotic symptoms, has helped educate the public about the medical nature of many psychiatric symptoms including mood and personality changes. These diagnoses have included herpes encephalitis, syphilis, hypercortisolism (Cushing’s), Wilson’s disease, hemochromatosis, and Korsakoff’s syndrome (vitamin B1 deficiency).
"Everybody Lies" conveys a message about stigma, false perceptions and misinformation about mental illness. In the TV show, the phrase represents that people who are being diagnosed with ANY illness often withhold information. In a time when it seems that Hollywood has been indifferent to, or even has propagated, stigma about mental illness, it is refreshing that the producers and cast of a TV show are helping to combat that.
NAMI executive director Mike Fitzpatrick says,
"On behalf of every individual and family who live with major depression, bipolar disorder, schizophrenia and other mental illnesses, NAMI thanks the show and cast. They are making a difference in people’s lives."
In addition to the sale of the T-shirts, an on-line auction is running for seven days (1 May 2007 through 7 May 2007) to sell five special autographed items. All proceeds go to NAMI.
Sage Words about Violence and Mental Illness
One of the blogs that I highlight down of the left-hand side of this one is attached to schizophrenia.com.
They have a particularly good entry for April 20th, that discusses not just the tragedy in Virginia and its possible relationship to mental illness, but also some broader social questions. Having been born and raised in the UK, and then worked there and in the United States in both medicine and psychiatry I can really relate to many of the points made in the article. It really should be disseminated as widely as possible, so I am going to do something that I usually do not, and quote the article in full:
The Loss of Life in Virginia, and How it Could Have Been Prevented
Read more… Schizophrenia, Poverty & CrimeWhenever a tragedy happens such as the recent shootings in Virginia,
the question inevitably turns to why did it happen, and how could it
have been prevented.While some reports (such as here, here and here)
have suggested the shooter in this tragedy – Cho Seung Hui – might have
suffered from psychotic depression, schizophrenia or bipolar disorder –
its impossible to know with the limited amount of evidence available,
and even after all the evidence is reviewed it will never be known for
sure.From what has been reported it does, however, seem obvious that he
was seriously depressed and socially withdrawn, and had some
significant delusions of persecution and paranoia. Whether these
symptoms add up to a serious mental illness or some type of sociopathic
disorder is unknown. Some factors don’t seem to point towards
schizophrenia – as Cho Seung Hui did not seem to suffer from the lack
of motivation (called avolition) that is so common with schizophrenia.
He was able to attend college and, from the sounds of things, was
attending classes regularly and finishing his assignments. Typically
when a person develops schizophrenia schoolwork and personal hygiene
the first thing that suffers, and an inability to complete schoolwork
is common.With regard to the question of why did it happen – it is of course
impossible to know for sure. But at the same time research into mental
illness and brain disorders does point to some possible answers.The path towards mental illness (any mental illness) is a complex
one with many different factors – from genetic predisposition and
pregnancy factors, to early life stresses and environmental factors, to
social stresses. We have more information on this in our “Preventing Schizophrenia”
– but fundamentally the factors that nudge people towards mental
illness are many and varied. The factors that have been conveyed about
the life of Cho Seung Hui suggest that early life experiences could
have been factors. Here are some of the relevant points that have been
discussed in the news:1. A Difficult Early Life – news on the family has suggested that
they had a difficult (low-income) family life in Korea which prompted
the move to the US when the parents had a young family. A low income
life that motivates a young family to leave a country – is likely to be
a high stress environment – a factor that could contribute to mental illness.2. Social stresses of immigration to the US (many studies out of the
UK have indicated that immigrants frequently face extremely difficult
social challenges in new countries due to a lack of understanding of
social norms (as well as racism) – which causes a great deal of social stress and significantly higher rates of mental illness.3. Cho Seung Hui’s Father worked in a Dry Cleaning company – and the family may have been exposed to higher levels of dry cleaning chemicals – which are linked to neurological damage.
Additionally, on a related topic, Dr. Michael Merzenich, the Neuroscientist at UCSF – comments in his blog
on the important issues related to the general social environment that
is also a factor in the extremely high levels of gun violence and
deaths in America – typically 300% to 600% higher than in other
developed countries:“Our jurisprudence is based on
the principle of “blame” for behaviors that should by hypothetically
controlled by our “free will”. Alas, human observers and psychologists
(and with increasing clarity, we brain scientists) have understood from
the beginning of time that your or my “will” is not entirely “free”.
The boundaries of “good judgment” are defined by a combination of the
inherited factors governing our brain function, by our physical brain
status (2 million head injuries/annum in the US alone!), and the
brain’s own plasticity-embedded experiences. For most of us, our
genetics combined with fortuitously not busting our skull in the wrong
place and with our particular plastic, experientially-driven brain
‘history’ adequately protects us from serious transgression. At the
same time, in our (and other) contemporary society(ies), we tolerate
conditions that result in millions of young men and women being reared
with an experiential history that is NOT adequate to keep THEM safe
from offending. THIS IS THE PART OF THE EQUATION THAT IS UNDER OUR
(SOCIETY’S) CONTROL. We’re doing a bad job with it. In fact:
1) We live in a violent society chock full of models of behavior (a
violence & fear-obsessed media, violent films, gangsta rap, et
alia) that are well outside any rational societal norms. The mass
murder of children on school campuses is one our MANY rather
spectacular modern American-violence inventions with little historical
precedent.2) We tolerate the hardening of young brains to
otherwise-not-tolerable bloody, shoot-em-/slash-em-up violence as an
acceptable source of intensive training “fun” in the heavily-rewarded
game-play of millions of our children. All that intensive training is
somehow supposed to be just fine for the child and their brain?! Those
tens or hundreds of thousands of violent repetitions in rewarded
behaviors just don’t matter a whit? Stuff and utter nonsense.3) We continue, collectively, to find innumerable ways to shame
children in their young lives as “failures”, “weaklings”, “misfits” or
“oddballs” in school and in life.4) We send juveniles and young adults off to crime school (prison) at an extraordinarily high (and growing) rate.
Sometimes I think that we could hardly be doing a better job of
training young people to misbehave. When they do, we hold them to a
universal high standard of acceptable behavior that they may actually
have had little experience with, in their own path through life, in our
very own society.”Lastly – there is the issue of easy access to guns in the US – which
when combined with all the above factors makes for an extremely toxic
mixture. Easy access to guns results in high death rates in shootings;
death rates that are typically 500% to 1,000% higher in the US than in
other civilized countries, as can be seen in the diagram below.National Comparisons for Selected Countries Homicide Rates Per 100,000 Population
Source: Corrections Service CanadaAs New Scientist Magazine notes
“Scientific studies have demonstrated over and over that owning a gun
makes it significantly more likely that you will be shot. The US has
the highest rate of firearms-related homicide in the industrialized
world – Americans are literally sacrificing hundreds of innocent
citizens each year upon the altar of the Second Amendment.”Are any of these factors preventable? Yes – of course they are – but
the actions are costly and complex. To prevent these types of tragedies
takes:1. Better education of the public about how to achieve mental health for their children,
2. Early and easy treatment for mental disorders with early testing and screening in schools,
3. Good insurance coverage
so that people can actually get their mental health problems addressed.
The US is the only developed country in the world that severely limits
coverage of mental health problems. Better and easier access to high
quality mental health treatments is a great need in the US.
4. Laws that make it possible for mentally ill people to get treatment, even though they may not understand the need.
5. A reduction in the culture of violence in the US (a movement to reduce violence in movies, on TV, and in video games). Read: In denial about on-screen violence for more information.
6. Strict gun controls
that take the millions of hand guns off US streets, and that will make
it more difficult for the people who become mentally ill or who have
psychiatric disorders – to obtain guns. Approximately 29,000 US
citizens are killed by their fellow citizens each year, by hand guns.
(see Statistics, Gun Control Issues, and Safety for more information)The answers are relatively clear – but whether we actually do anything about it is up to you.
Related Reading:
Mental Health, the Law and Predicting Violence (NPR)
America’s tragedy – Its politicians are still running away from a debate about guns (The Economist)
Mayors urge Bush to tighten gun control laws
Stricter gun control after shootings at U.S. university – not going anywhere fast
Relationship of US gun culture to violence ill-understood
Violence may be a ‘socially infectious disease’
Madness and Genius Revisited
I must have heard a thousand times that there’s a fine line between genius and insanity. I have talked before about the possible link between the two through schizotypal personality disorder. It is quite well known that there are two living Nobel Prize winners who have a diagnosis of schizophrenia and many more who have first-degree relatives with it.
There is some very interesting research in the current issue of the Journal of Clinical Investigation from a team of scientists at the National Institutes of Health’s (NIH) National Institute of Mental Health (NIMH).
In the latest installment of a story that has been unfolding over the last three decades, they report on their findings concerning a human gene for a master switch in the brain called DARPP-32. Most people inherit a version of a gene that optimizes their brain’s thinking circuitry, yet paradoxically also appears to increase risk for schizophrenia, an illness marked by impaired thinking. The main kinds of thinking involve reasoning, abstraction and creativity.
Over the last two decades, studies in animals, most notably by Nobel Laureate Paul Greengard at Rockefeller University, have established that DARPP-32 in the striatum switches streams of information coming from multiple brain chemical systems so that the cortex can process them. Both the neurotransmitter that DARPP-32 works through – dopamine – and the chromosomal site of the DARPP-32 gene have been implicated in schizophrenia.
The NIMH researchers in this new study have identified a common version of the gene and showed how it impacts the way in which two key brain regions exchange information, so affecting a range of functions from general intelligence to attention.
To understand DARPP-32’s role in the human brain, they used genetic, structural and functional magnetic resonance imaging and also post-mortem studies to identify the human gene’s variants and their functional consequences.
Seventy five percent of subjects had the most common version of the gene, which boosted the activity of circuits in the prefrontal cortex of the brain. This region is the major filter, controller and processor of cognitive information. When active, it increases structural and functional connections and our performance on tasks that involve thinking. It almost certainly does so by increasing gene expression. In 257 affected families, people with schizophrenia were also more likely to have this common version of the DARPP-32 gene.
DARPP-32 appears to shape and control a circuit running between the striatum and prefrontal cortex. The circuit affects key brain functions implicated in schizophrenia, such as motivation, working memory and reward-related learning.
The senior investigator is Daniel Weinberger, who had this to say,
"Our results raise the question of whether a gene variant favored by evolution, that would normally confer advantage, may translate into a disadvantage if the prefrontal cortex is impaired, as in schizophrenia. Normally, enhanced cortex connectivity with the striatum would provide increased flexibility, working memory capacity and executive control. But if other genes and environmental events conspire to render the cortex incapable of handling such information, it could backfire — resulting in the neural equivalent of a superhighway to a dead-end."
Although several groups of researchers have looked for the possible clinical relevance of DARPP-32, they have had much success. This study shows a strong connection between the molecule and human cognition and also, perhaps, with schizophrenia.
What is also interesting about this finding is that it helps provide us with a mechanism by which environmental stress could lead to cognitive problems.
Apart from the uninformed tirades of Tom Cruise, I see a lot of opinion pieces on websites and YouTube expressing the opinion that psychiatry is baseless, ostensibly because there is no science behind it. By anyone’s standards, this is high level science utilizing a series of state-of-the-art approaches. And another piece of evidence that psychiatry is becoming more science than art, linking the mind, the brain and the environment into one harmonious whole.
Hormones, Addictions and Mood

People working with mental illness have been for years now been puzzled by two observations. The first is that mood disorders and schizophrenia follow quite different trajectories in men and women. Women tend to be more vulnerable to mood disorders and if they get schizophrenia it tends to be less severe and to have fewer “negative” symptoms, such as flat, blunted or constricted affect and emotion, poverty of speech and lack of motivation until after menopause. We have looked at some of the reasons for the different rates of mood disorder, in terms of relationships and social pressures, but there must also be a biological component. The second puzzle is that women are more vulnerable to addictive drugs in the days before they ovulate.
New research published in the Proceedings of the National Academy of Sciences may provide part of the answer to both puzzles.
Colleagues at the National Institute of Mental Health (NIMH), a component of the National Institutes of Health (NIH), have conducted a fascinating imaging study that has shown that fluctuations in levels of sex hormones during women’s menstrual cycles affect the responsiveness of the reward systems in the brain.
The reward system circuits include the:
- Prefrontal cortex, which has key roles in thinking, planning and in the control of our emotions and impulses
- Amygdala, which is involved in rapid and intense emotional reactions and the formation of emotional memories
- Hippocampus, which is involved in learning, memory and navigation
- Striatum that relays signals from these areas to the cerebral cortex
It has been known for some time that neurons in the reward circuits are rich in estrogen and progesterone receptors. However, how these hormones influence reward circuit activity in humans has remained unclear.
The researchers used functional magnetic resonance (fMRI) imaging to examine brain activity of 13 women and 13 men while they performed a task that involved simulated slot machines. The women were scanned while they did the task, both before and after ovulation.
When anticipating a reward, in the pre-ovulation phase of their menstrual cycles the women showed more activity in the amygdala and frontal cortex. When women were actually winning prizes, their reward systems were more active if they were in the phase of their menstrual cycle preceding ovulation. This phase of the cycle is dominated by estrogen, compared to postovulatory phase when estrogen and progesterone are both present. When winning, the main systems that became active were in the parts of the brain involved in pleasure and reward.
The researchers also demonstrated that the reward-related brain activity was directly linked to levels of sex hormones. Activity in the amygdala and hippocampus was in directly linked to estrogen levels, regardless of where a woman was in her cycle. When women won prizes during the post-ovulatory phase of the cycle, progesterone modulated the effect of estrogen on the reward circuit.
Men showed a different activation profile from women during both anticipation and delivery of rewards. Men had more activity in the striatum during anticipation compared with women. On the other hand, women had more activity in a frontal cortex when they won prizes.
This research could have a number of important implications. The most obvious is that it confirms what many women know already: they are more likely to take addictive substances or to engage in pleasurable – but perhaps impulsive or risky – behaviors just before they ovulate.
It is not difficult to imagine why this might have developed during evolution.
“Coming to terms with the rhythms of women’s lives means coming to terms with life itself, accepting the imperatives of the body rather than the imperatives of an artificial, man-made, perhaps transcendentally beautiful civilization. Emphasis on the male work-rhythm is an emphasis on infinite possibilities; emphasis on the female rhythms is an emphasis on a defined pattern, on limitation.”
–Margaret Mead (American Anthropologist and Writer, 1901-1978)