More Genes Involved in Obesity

I am impressed by the progress being made by some of my former colleagues who are busily unraveling the complex genetics of obesity.
In a paper in the journal Science a group of British scientists including Chris Ponting of the Medical Research Council Functional Genetics Unit in Oxford and Stephen O’Rahilly’s group at the University of Cambridge, has made a second breakthrough in twelve months in understanding how a gene triggers weight gain in some individuals. In May we looked at the first piece of work on the gene called “FTO.”
At that time we learned that variations in the FTO gene influence people’s risk of becoming obese. This particular gene was of great interest because the genetic variant in FTO that predisposes to obesity is very common in the population.
About half the British population carries a copy of the variant and they are on average 3-4 pounds heaver than those who do not have it. The 16 per cent of the population who carry two copies of the variant and are on average 6-7 pounds heavier. We also learned that carriers of the variant have an increased risk of diabetes. However the function of FTO was completely unknown.
The new paper shows that the FTO gene codes for an enzyme – 2-Oxoglutarate-Dependent Nucleic Acid Demethylase – that can act directly on DNA. This strongly suggests that FTO might have a role in controlling how and when genes are turned on and off.
The investigators also found that FTO is highly expressed in the hypothalamic region of the brain, which has important roles in the control of hunger and satiety. In certain areas of the hypothalamus, the levels of FTO are influenced by feeding and fasting.
This is a remarkable finding. That a gene involved in obesity and diabetes has a direct effect on DNA in specific regions of the brain is very exciting. It suggests that the gene is involved in influencing how well the brain senses hunger and fullness. Small molecules derived from metabolism can modulate the activity of FTO, so we can see a direct link form food to metabolism to DNA in the brain.
The findings raise all kinds of treatment possibilities and also confirm something that I have been teaching for three decades: weight control does not start with a diet. It starts between the ears. Until you have been shown how to re-program your brain, thoughts and emotions, your chance of successfully controlling your weight is, ahem, slim.
Nutrition and Female Fertility

Whoever said that “you are what you eat” was not wrong. The composition of our diets can affect everything from our moods to our risk of getting some types of cancer.
Now it looks as if nutrition may also be an essential part of helping at least one type of infertility.
There are literally hundreds of causes of infertility, but one of the more common ones in women is a problem with ovulation. A rapidly growing cause of ovulatory problems is the polycystic ovarian syndrome, which is itself associated with insulin resistance.
New research from Harvard School of Public Health is published today in the prestigious journal Obstetrics & Gynecology which suggests that women who followed a combination of five or more lifestyle factors, including changing specific aspects of their diets, had more than 80 percent less relative risk of infertility due to ovulatory disorders when compared with women on more unhealthy diets.
The investigators followed a group of 17,544 married women who were participating in the Nurses’ Health Study II, which is based at the Brigham and Women’s Hospital in Boston. The researchers created a scoring system on dietary and lifestyle factors that previous studies have found to predict ovulatory disorder infertility. Among those factors were:
- The ratio of mono-unsaturated to trans fats in diet
- Consumption of animal or vegetable protein consumption
- Carbohydrates consumption, which included both dietary fiber the glycemic index of foods
- Dairy consumption: both low- and high-fat
- Iron consumption
- Multivitamin use
- Body mass index
- Level of physical activity
The researchers then assigned a “fertility diet” score of one to five points. The higher the score, the lower the risk of infertility associated with ovulatory disorders.
The women with the highest fertility diet scores ate:
- Less trans fat
- Less sugar from simple carbohydrates
- More vegetable than animal protein
- More fiber and iron
- More multivitamins
- More high-fat dairy products and less low-fat dairy products
The more fertile women also had a lower BMI and exercised for longer periods of time each day.
This relationship between a higher “fertility diet” score and lesser risk for infertility was similar for different subgroups of women. It seemed to hold in many different age groups, and whether or not a woman had been pregnant in the past.
The effect size is impressive: women following five or more low-risk dietary and lifestyle habits have a six fold reduction in ovulatory infertility risk compared with women following none of them.
There are two surprises here. It has been believed that heavier – though not obese – women tended to be more fertile. That is not what this study found. Second, the higher fertility rates of women who consume high-fat dairy products and less low-fat dairy products may seem counter-intuitive. But well-nourished women would be expected to have a higher chance of being fertile.
The take home message is this: if a woman is having problems with ovulation, sensible dietary choices and a moderate amount of physical activity may make a large difference in her chance of becoming fertile.
This all makes sense. From an evolutionary perspective it could be dangerous to bear a child while ingesting foods, chemical or toxins that could harm a baby, or could compromise the health of a pregnant mother.
“Nutrition can be compared with a chain in which all essential items are separate links. We know what happens if one link of a chain is weak or is missing. The whole chain falls apart.”
–Patrick Wright (American Director of the Institute for Research on Food-related Disease)
“Health requires healthy food.”
–Roger Williams (Indian-born American Chemist who did pioneering work on the Vitamin B Complex, 1893-1988)
The Evolving Obesity Pandemic
Here is something that is not too much of a shock. At least it isn’t until you look at the numbers.
People are getting heavier throughout the world, with the possible exception of south and east Asia. These are the conclusions of a one-day global “snapshot:” a single day in 2006 when doctors and nurses in 63 countries across five continents – not even including the United States – found that between half and two-thirds of men and women in were overweight or obese.
The study is being published in the journal Circulation and included 168,159 people. The initial results were published http://eurheartjsupp.oxfordjournals.org/cgi/content/abstract/8/suppl_B/B26 last year in the European Heart Journal, but this new report puts more “flesh” on the original report.
The International Day for the Evaluation of Obesity (IDEA) study looked at two measures of fatness – waist circumference and body mass index or BMI.
A BMI (weight in kg divided by square of height in meters) of 18.5 to 25 is considered healthy. A BMI over 25 is considered overweight and greater than 30 is obese. I shall have something to say about BMI in a moment.
In Eastern Asia 7% were obese, compared with:
- 36% of people in Canada
- 38% of women in Middle Eastern countries
- 40% in South Africa
Canada and South Africa led in the percentage of overweight people, with an average BMI of 29 among both men and women in Canada and 29 among South African women.
In Northern Europe men had an average BMI of 27 and women 26. In other words they were just into the overweight “category.” In southern Europe, the average BMI was 28. In Australia BMI for men was 28 and 27.5 for women. In Latin America the average BMI was just under 28.
Waist circumference was also high – 56% of men and 71% of women carried too much weight around their middle.
The overall frequency of heart disease was 16% in men and 13% in women. In Eastern European men, many of whom still smoke, the rates of heart disease, 27%, and women, 24%. By comparison in Canada the rate of heart disease in women was 8%, and in men 16%.
The rates of diabetes varied across regions. Overall, 13% of men and 11% of women were diagnosed with diabetes.
This means that the rest of the world is catching up with the United States, long considered the country with the worst weight problem.
An estimated two-thirds of Americans are overweight and a third of these are obese. In the US, the lifetime risk of developing diabetes, is also high – 33% for men and 38% for women.
In studies like these, a BMI over 25 is considered to be overweight and greater than 30 is obese. I have commented before about the limitations of using BMI, but it remains a way of getting an overall picture of what is happening in the body.
The findings are deeply worrying.
It is well known that increasing weight, particularly the amount of fat carried inside the abdomen – not the “lovers’ handles!” – increase the risk of coronary artery disease, Type II diabetes and other diseases including some cancers. That point about the “intra-abdominal” fat I all important. For years we have been told that even small increases in weight can do us harm, but that is not completely accurate. It is where the fat is deposited, not only how much we have. It is only when people become extremely obese all over that the risks of many diseases begin to climb.
The moral of the story?
Watch you the size of your abdomen, and stay tuned as I give you more advice about the Whole Person ways to control you weight.
Dopamine, Drugs and Diabetes
We recently talked about the increasing evidence that insulin has many extremely important roles in the brain.
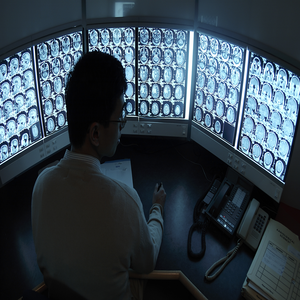
New research by investigators at the Center for Molecular Neuroscience and the Institute of Imaging Science at Vanderbilt University Medical Center researchers, working with colleagues in Texas, has found that insulin levels affect the brain’s dopamine systems. These systems are involved in motivation, reward, salience, movement and emotional processing. Disturbances in dopamine pathways have been implicated in substance abuse, as well as schizophrenia, bipolar disorder and attention deficit hyperactivity disorder (ADHD). Drugs that interfere with the dopamine pathways may produce Parkinsonism as well as elevations of the hormone prolactin.
The psychostimulant drugs amphetamine and cocaine, as well as related medications for ADHD, block the reuptake of the neurotransmitter dopamine by dopamine transporters (DATs) thereby increasing the level of dopamine signaling. Some of these compounds also cause a massive surge of dopamine through DATs, resulting in high levels of synaptic dopamine that alter attention, increases motor activity and plays an important role in the addictive properties of psychostimulants.
The reason for examining a possible relationship between dopamine and insulin goes back to the 1970s, when it was reported that amphetamine had no effect on diabetic animals and in the 1980s it was shown that diabetic rats did not show the usual stereotyped behaviors when given amphetamine. There were also odd reports about disturbances in the enzyme dopamine-beta-hydroxylase in experimental diabetes and changes in dopamine D1 receptors in the brains of rats with induced diabetes.
These observations lead to this new research into a possible link between insulin signaling and amphetamine action.
They used a standard a rat model of type 1 diabetes in which insulin levels are massively depleted, and then assessed the function of the dopaminergic pathway in the striatum, an area of the brain rich in dopamine.
In the absence of insulin, amphetamine-induced dopamine signaling was disrupted: dopamine release in the striatum was severely impaired and expression of DAT on the surface of the nerve terminal was significantly reduced.
The lack of the DAT protein on the plasma membrane prevents the amphetamine-induced increase in extracellular dopamine, and in turn, amphetamine fails to activate the dopamine pathways that stimulate reward, attention and movement.
The researchers then gave insulin into the brains of the diabetic animals and found that the system returns to normal, indicating that the lack of insulin in the striatum directly affected amphetamine action.
They also developed a probe for brain DAT activity using functional magnetic resonance imaging (fMRI). In normal, healthy rats with plenty of insulin, amphetamine increased neural activity in the striatum. But in diabetic animals, activity in the striatum was suppressed.
So there is a powerful interplay between dopamine neurotransmitter systems and insulin signaling mechanisms. The results are some of the first to link insulin levels and dopamine function in the brain and hold several implications for human health and disease.
We need to have another look at the effect of diabetes on the brain. We have known that people with diabetes are at increased risk of cognitive impairment and depression, and we had assumed that it was because of hypoglycemia and vascular disease. Those assumptions may have been wrong.
The findings may also be important for diseases with altered dopamine signaling, such as schizophrenia and ADHD. Insulin may have something to do with the underlying brain disturbances in ADHD. Then control of insulin levels and neuronal responses to the hormone may help determine the efficacy of psychostimulants in people with ADHD.
Every now and then you see people on psychostimulant medications who need huge doses. Perhaps their problem lies with insulin rather than dopamine.
Alzheimer’s Disease: Diabetes of the Third Kind?

Insulin may have some extremely important roles in the mind as well as the body.
Though best known for its role in promoting glucose uptake into cells, insulin has at least five hundred known functions in the human body. For many years nobody was sure whether insulin was important to the brain: neurons in the brain are unusual in that they do not need insulin to enter them. But then we discovered that insulin acts on other important metabolic processes in neurons. In the brain it also does duty as a chemical messenger and as a growth factor, and brain insulin signaling is crucial for the creation of memory. Over the years a number of theorists have suggested that some neurological and psychiatric illnesses could be a result of disturbances in insulin-related processes in the brain.
It is now beginning to look as if they may have been correct.
Some recent evidence has suggested that Alzheimer’s disease and diabetes mellitus share a number of common pathways and Alzheimer’s disease is associated with peripheral insulin resistance.
New research has been published by investigators from Northwestern University in the FASEB Journal – the journal of the Federation of American Societies for Experimental Biology – that may finally nail down the reason why insulin signaling may stop working in Alzheimer’s disease.
The research team used mature cultures of neurons from the hippocampus of the brain to study synapses – the connection between neurons – that have been implicated in learning and memory mechanisms. They wanted to examine the effect of a toxic protein, known to attack memory-forming synapses, that is called “ADDL” for “amyloid ß-derived diffusible ligand.” ADDLS are small, soluble aggregated proteins that accumulate in the earliest stages of Alzheimer’s disease. The researchers had previously found that ADDLs bind very specifically at synapses, which in turn initiates deterioration of their function, shape and composition. They now went on and studied the synapses and their insulin receptors before and after ADDLs were introduced. Regions of the nerve with normal numbers of insulin receptors have no ADDL binding, but when the ADDLs are added they remove insulin receptors from nerve cells, effectively making them insulin resistant.
And an insulin resistant neuron cannot participate in the formation of memories.
This finding implies that there is a fundamental connection between diabetes and Alzheimer’s disease, and this may in turn help us to see whether existing diabetes treatments might protect neurons from ADDLs and improve insulin signaling in people with Alzheimer’s disease.
The first type of diabetes is Type 1, a.k.a. insulin-dependent or juvenile onset. The second is Type 2, a.k.a. non-insulin-dependent diabetes. So is Alzheimer’s Type 3?
It has also been known for some time that physical exercise is one of the factors that may help reduce the chance of developing Alzheimer’s disease, and we may now have a mechanism by which it can help.
This is an extraordinarily interesting and important discovery that should lead to a whole new research angle, perhaps with medicines that are already available.
Diabetes, Inflammation and the Heart

One of the most worrying signs in people with type 1 diabetes is damage to the nerves supplying the heart. This is called cardiovascular autonomic neuropathy, and one of its first signs is a reduction in the normal heart rate variability (HRV).
It has been known for many years that people with both type 1 and type 2 diabetes have low grade inflammation, and inflammation can have profound effects on the activity of the autonomic nervous system.
A study from Sabadell in Spain has tried to sort out these links in a study of 120 people with longstanding type 1 diabetes.
They measured a great many things including tumor necrosis factor, alpha-receptors 1 and 2, IL-6, and C-reactive protein; insulin resistance and HRV in response to deep breathing and the Valsalva maneuver” forcibly exhaling against with mouth and nose closed.
They did indeed find a link between low-grade inflammation and early alterations in the nerve supply to the heart.
This is important information: when we proposed that inflammation might be an important player in diabetes back in the 1980s, it was greeted with disbelief. Twenty years on it looks as if we might have a whole new line of treatment on the horizon, which will include nutrition and exercise as well as supplements and medications.
Insulin Resistance and Cognition
I have talked a lot about insulin resistance and the problems that it can cause. It is one of the biggest threats facing the human population, with at least a third of Americans now being insulin resistant. It looks as there may be another complication of insulin resistance that we need to add to the list.
Researchers from Canada presented some interesting data (NR385) at the 2007 Annual Meeting of the American Psychiatric Association in San Diego last month.
There has been a great deal of concern that some newer antipsychotics may cause insulin resistance and perhaps diabetes, and the FDA has required all the newer antipsychotics to carry a warning about this potential problem. We also know that although these medicines can be very effective in treating some symptoms, they do not usually help cognition very much.
The researchers recruited 37 people with chronic schizophrenia and did neurocognitive tests on them while also measuring their insulin resistance.
They found a significant correlation between insulin resistance and neurocognitive functioning. It looks as if insulin signaling is important for processing information in the brain and insulin resistance interferes with the process.
Though this study look at a highly specialized group: people with chronic schizophrenia – there is some recent evidence to suggest that insulin resistance may be a factor in Alzheimer’s disease, and that people may develop cognitive impairments if they go on to develop insulin resistance syndrome or impaired fasting glucose.
Yet another good reason for using diet, exercise and sleep to try and present insulin resistance and maintain healthy glucose levels.
Regular readers will recall that there are five pillars of healthy aging and the prevention of cognitive decline:
- Blood pressure
- Physical activity
- Mental activity
- Supplements and moderate alcohol
- Social engagement and level mood
We should now add avoidance of insulin resistance to the list. Taken together, the evidence suggests that we can dramatically reduce our risk of cognitive decline as we get older.
Half the Population Has Genes to Make Them Fat

I have talked a bit about my skepticism concerning the genetic contribution to obesity, insulin resistance and diabetes.
I was fascinated to see a huge fifteen year study that has just been published in the journal Science. I felt a touch of pride: back when the earth was new, I helped train more than one of the authors.
The study involved over 42,000 people and found an association with body mass index at every age [from seven to 70] in populations throughout the UK and Europe.
Unlike previous work, it shows a very common genetic link with mild obesity rather than a rare genetic link with extreme obesity.
There were 42 scientists in the group and they found that if people carry one copy of a variant in a gene called FTO, as does half of the general population, it will lead to a gain in weight of 2.6lb or put just over half an inch on their waists and raise their risk of being obese by one third. People with two copies of this variant in the FTO gene, which is the case in one in six of the population, then they will gain almost 7lb more than those who lack the variation and are at a 70 per cent higher risk of obesity.
The researchers then tested a further 37,000 people from Bristol, Dundee and Exeter as well as a number of other regions in Britain, Italy and Finland. In every case the same variant in the FTO gene – which is mostly present in the brain and pancreas, among other key tissues – was associated with type 2 diabetes and obesity.
They also showed that in children, this particular FTO variant was associated with increased body weight.
We hope that in the future, once we have found additional obesity genes, it may be possible to offer advice based on a person’s genetic make-up. We all know that folk are eating more and doing less exercise, but some people gain more weight than others. Similarly two people on the same diet and exercise plan lose different amounts of weight. There are undoubtedly some unrecognized factors in weight gain, but genes remain in the mix.
Never be disheartened if your first attempt at diet and exercise is not crowned with success: they are only two of a dozen factors that play into weight control.
Do not fall into the fatalistic trap of thinking that biology is destiny.
We are talking about a factor that may modulate the way in which we control out weight.
As promised, I shall soon be publishing a book detailing specific methods for dealing with whichever ones are important in your life.
Your future lies in your hands: not in a string of chemicals.
The Causes and Consequences of Insulin Resistance
I have spent so much time talking about insulin resistance becuase it is one of the greatest medical threats facing the world.
It is estimated that approximately 33% of the adult population of the United States is insulin resistant, and if left untreated many will develop diabetes, hypertension and an array of other problems. It is an epidemic that is expected to swamp most health care systems around the world, yet sadly it may in most cases be preventable.
There is an enormous literature on insulin resistance. As of this afternoon there are almost 33,000 scientific papers on the subject.
I created this graphic to try and summarize the key points about insulin resistance: the main factors that may cause it, as well as the most important medical consequences.

(Click on the graphic to expand it.)
The Main Causes of Insulin Resistance are:
- Aging
- Intra-abdominal obesity
- Inactivity
- Glucose intolerance
- Genetics
- Fetal malnutrition
- Cigarette smoking
- Some medications
The Main Consequences of Insulin Resistance are:
- Type 2 diabetes mellitus
- Hypertension
- Arteriosclerosis
- Polycystic ovarian syndrome
- Non alcoholic fatty liver disease
- Disturbances in the function of the vascular endothelium
- Elevations of triglycerides and cholesterol
- Disturbances of clotting
- Disturnaces in kidney function
- DIsturbances in one type of heart rhythm
- Elevated uric acide levels
- Some malignancies
This is probably not a complete list, but it gives you a very good idea of the reasons for looking for insulin resistance. Many – but not all – experts now recommend measuring insulin resistance in people at high risk of developing any of these medical problems.
We have good evidence that lifestyle changes can prevent the development of many of these dire consequences, so it is certainly something worth discussing with your health care provider.







