Farmer P.
Well today your humble reporter is like a dog with two tails.
He has never tried growing anything other than roses and herbs, but She Who Must Be Obeyed wanted vegetables. So I was dispatched to create a vegetable garden. Being in the American colonies, we decided to use the old Native American method, planting corn, squash and beans in the same hole in the ground, so that the corn grows, providing a climbing structure for the beans, and the two together provide shade for the squash. Being originally of an English persuasion, I hadn’t seen squash, except as an occasional import in exotic stores, so I didn’t know what to expect.
Well here is my first crop.
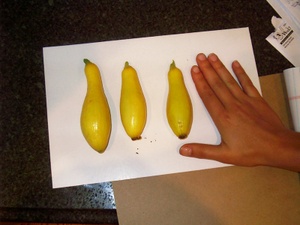
Thank you to Morgan Wenner for providing her hand!
I am now in the market for squash recipes: I think that we’re going to be living on them for a while….
Sleep, Weight, Insulin Resistance and Diabetes
I am often asked why there seem to be such close links between food and mood. Not just comfort eating, or the sudden shock of lots of carbs when we need an energy jolt, but why drugs that alter mood so often alter appetite?
You will probably not know this, gentle reader, but I only learned of it from reading scholarly papers. Apparently many people report that using marijuana makes them very hungry. On the other hand, cocaine and amphetamine affect not just the metabolism, but also appetite. The link has to do with the evolutionary development of feeding behaviors with the motivation to find food and to be satisfied by it.
Another link that has interested me for many years is the connection between metabolism and sleep. We have always presumed that this link has to do with hibernation: even humans have maintained some hibernation responses.
There is extremely good evidence that there is an inverse relationship between the number of hours that you sleep and an increase in your weight. There have been a great many studies on this, but one of the best was published by a group of researchers from the Mood and Anxiety Disorders Program, at the National Institute of Mental Health, the Psychiatric University Hospital, Zurich, Switzerland; University of Pittsburgh School of Medicine and the Department of Psychosocial Medicine, Zürich University Hospital, Switzerland in the Journal Sleep in 2004.
A report from the BBC concerning a study presented to the American Thoracic Society International Conference in San Diego provides yet more evidence of this link between sleep and weight. Researchers from Case Western Reserve University in Ohio, followed nearly 70,000 women for 16 years. They found that women who slept five or fewer hours a night were a third more likely to put on at least 33lbs (15kg) than sound sleepers during that time. It also found that compared with women who slept for seven hours a night. lighter sleepers were 15% more likely to become obese (have a Body Mass Index (BMI) of 30 or more. {BMI is calculated by dividing your weight in kilograms by the square of your height in meters}).
Previous studies, some of which I have reported before, have shown that after just a few days of sleep restriction, the hormones that control appetite cause people to become hungrier. However the women in the study appeared to eat less. I say “appeared to,” since the use of personal evaluations of food intake are notoriously inaccurate.
In dozens of countries arond the world, I am regarded as an authority in the fields of endocrinology, metabolism and nutrition. But when a group of us tried to estimate our daily intake and compare it with meticulous diaries, we discovered that we – a group of internationally renowned experts – were off by around 500 calories per day.
All kinds of explanations have been advanced, from people who didn’t sleep getting up and binge eating; to the effects of sleep-deprived people craving high carbohydrate, high fat food; to insomnia being a result of anxiety or depression that releases hormones that cause us to lay down fat in our tummies.
For all kinds of complex biochemical reasons, I have always felt that a lack of sleep would lead to an increase in insulin resistance, that may cause an increase in the deposition of fat in key regions of the body.
Some new research suggests that I may have been right on this one. A group based at Yale University School of Medicine, in New Haven, Connecticut has just published a report that should be of interest to all of us, and in particular you multi-tasking insomniacs out there.
The investigators studied a cohort of men from the Massachusetts Male Aging Study who did not have diabetes at baseline (1987–1989) and who were followed until 2004 to look for the development of diabetes mellitus. They came to the conclusion that BOTH very short and extra long sleep durations increase the risk of developing diabetes, independent of confounding factors.
The take home message?
If you do not get 7-8 hours sleep each night, you are vulnerable to a great many problems, and perhaps the biggest of all is the risk of weight gain, insulin resistance and diabetes mellitus.
I do not recommend using sleeping tablets unless absolutely necessary, and then for just a few days at a time. Instead follow all the sleep strategies that I have talked about in earlier blog entries.
During a recent visit to Danville, Virginia, I was delighted to learn that one of the non-pharmacological approaches that I have found helpful – putting a cold compress on the abdomen – was used by General Stonewall Jackson who used this very technique that I had to learn by going all the way to China.
The bottom line? Before your sleep gets disrupted by being overweight and you develop sleep apnea, try some simple sleep hygiene, and a few of these novel techniques.
Technorati tags: Insulin Insulin resistance Insulin resistance syndrome insomnia alternative medicine resilience
More on the Neurology of Obesity
The last year has seen a mass of new obesity research linking intestinal hormones and the brain.
Over the last 25 years, there has been increasing evidence that many people with significant weight problems have problems in a region of the brain called the hypothalamus that is involved in the control of appetite, feeding, temperature and a range of other bodily functions. On April 18th, I mentioned the intriguing possibility that viruses could be one previously unrecognized explanation for the obesity pandemic. It is hypothesized that these viruses might alter the normal functioning of the hypothalamus, causing an increase in feeding, and perhaps also of appetite and inactivity.
A study from Albert Einstein Medical College in New York, published in this month’s Journal of Clinical Investigation provides further evidence that there may be something wrong with the normal functioning of the hypothalamus.
We normally have a sensitive mechanism in the hypothalamus for sensing fats, which provide a strong signal to stop eating and also to start normalizing blood glucose. There are strains of obese rats, and in these little creatures the fat sensing mechanisms do not work properly. Not only do they keep eating, but also they cannot control their blood glucose properly. Those two things together conspire to produce yet more obesity. What was so interesting in this study, was that the researchers found that if they inhibited a single enzyme involved in fat metabolism, the levels of fatty acids rose in the hypothalamus, the animals were once again able to sense fat levels, and both their feeding and glucose levels normalized.
This is one of the first times that it has been possible to find a single enzyme that would normalize metabolism. The next question is to see whether this might constitute a viable treatment for obesity, or if the body would quickly work around the treatment and return to its old ways.
Technorati tags: weight control hypothalamus obesity
More Advances in Understanding Weight Control
I have on many occasions discussed the problem of over-simplifying the mechanisms controlling our weight and appetite. They are complex and have multiple fail-safes and multiple levels of redundancy, which is why most weight loss programs only last for short periods of time. The body gets used to the diet, believes that it is starving, and immediately gets to work to conserve energy: our metabolism slows and our physical activity levels begin to fall.
We can tinker with leptin, cortisol or insulin to our hearts’ content, and each will probably help for a while. But if we ignore the body’s starvation-protection mechanisms, to say nothing of the psychological, social and subtle aspects of weight, our efforts will usually be fairly short-lived. Most of us now understand that food intake is only part of the equation; we also need to maximize our metabolic rate and increase our level of physical activity. One of the problems has been how to help someone exercise whose body wants to go into starvation mode.
Steve Bloom’s group at Imperial College and the Hammersmith Hospital in London has published another valuable report helping to elucidate some of the complex mechanisms involved in appetite, weight and metabolism. Steve has been working in this area since the early 1970s, and is one of the most highly cited scientists in the world. In a field that constantly sees new discoveries replacing the old, he is unusual in that that virtually all of his work has stood the test of time.
This report concerns the intestinal hormone oxyntomodulin, which has a dual action, increasing energy expenditure as well as reducing food intake. It appears that oxyntomodulin may let the brain know it has an adequate energy supply and that it can afford to do productive things rather than just concentrating on food seeking behaviors or energy conservation. The hormone signals the brain that it can increase exercise by letting it know that the energy is available to do so.
At the moment oxyntomodulin has to be given by injection, and, given the complexity of the weight maintenance systems it is unlikely to be the whole answer.
Technorati tags: weight control obesity oxyntomodulin energy expenditure weight management
Viruses and Weight Gain
Another discussion in Healing, Meaning and Purpose revolved around the evidence that in addition to toxins, viruses have been attracting a great deal of attention as causative agents of obesity in humans. There are currently seven viruses known to cause obesity in animals and three in humans. This work began almost twenty years ago when a Dr. Nikhil Dhurandhar was working in India and discovered that viruses could cause obesity. It started with a chance observation: thousands of chickens were dying, and when they did, they were found to be abnormally heavy. He then discovered that people who had been exposed to a chicken adenovirus called SMAM-1 were consistently fatter than those who had had no exposure. He later moved to the U.S., and has collaborated with other researchers to study whether human adenoviruses, which are common throughout the human population, could be having a similar effect. This led to the discovery that the human adenovirus Ad-36 caused significant fat increases in animals, and furthermore was associated with obesity in humans. Now we have a new report from Leah Whigham and her team at the University of Wisconsin in Madison who tested several human adenoviruses for their ability to increase fat in both live chickens and in cell culture.
It is not at all far-fetched to suggest that there may in the future be vaccines to prevent one of the many causes of obesity. But for now, follow simple rules of hygiene and do everything that you can to improve your own resistance to infection. Which gets us straight back to Healing, Meaning and Purpose!
Technorati tags: weight gain, Nikhil Dhurandhar, virus,
Calcium, Vitamin D, Diabetes and Schizophrenia
There are some odd puzzles in medicine. For more than 100 years it has been known that diabetes is more common in people suffering from schizophrenia, bipolar disorder and probably also depression. There has also been data indicating that some children with ADD and autism have metabolic disturbances that may underlie some of the cognitive difficulties. It has also been observed in Europe that dark skinned immigrants – whose skin coloring makes them less able to make Vitamin D – are more likely to develop diabetes. Some dark skinned immigrants are also far more likely to develop schizophrenia compared with their families that stayed in sunny tropical regions. Children – particularly boys – who are breastfed and/or have Vitamin D supplements in the first year of life are less likely to develop schizophrenia in later life. Vitamin D is not only involved in calcium absorption, but also in maintaining the integrity of cell membranes. So the link between diabetes and schizophrenia may have something to do with Vitamin D.
A new study just published in the journal Diabetes Care indicates that women with high intakes of vitamin D and calcium appear to have a lower risk of developing type 2 (maturity onset) diabetes. The study from Tufts-New England Medical Center looked at data on 83,779 women enrolled in the Nurses’ Health Study. The women had no history of diabetes, cardiovascular disease or cancer when they enrolled in the study. Vitamin D and calcium intake from foods and from supplements were evaluated every 2 to 4 years. Over the 20 years of follow-up a total of 4843 new cases of diabetes were discovered. The lowest risk of diabetes was observed among women with the highest combined intakes of calcium and vitamin D compared with those with the lowest.
These are important findings, because interventions to raise both vitamin D and calcium intake and quick, cheap and easy, and may significantly reduce the risk of developing type 2 diabetes.
So how much should we take? Although we should be able to make enough of our own Vitamin D by spending even ten minutes in the sun, not everyone can do that, the sun is not without its risks, and the mechanisms for making Vitamin D become less effective as we become older. Though a balanced diet should also help provide some vitamin D and enough calcium, the data indicates that we should take in at least 1200mg of calcium each day, and 400 International Units (10 micrograms) Vitamin D each day. It is possible, though uncommon for people to take too much Vitamin D, and that can have all manner of health consequences.
Technorati tags: vitamins, diabetes, schizophrenia, calcium, Vitamin D,
Personal Evaluation of Wellness
As a physician, I am trained to know what questions to ask in order to diagnose health problems and understand what course of action needs to be prescribed to alleviate or cure the problem. I can be a nightmare for my secretary if she makes my schedule tight because I can spend over an hour with a patient on a first visit. She would argue that it is more like two hours, but I will admit that I take whatever time I need to gather the pertinent information.
I recently wrote an article that allows one to conduct a personal evaluation of his or her own wellness. Click here to be taken to it. It is based on my many years of experience and research. You will notice that the questions cover the 5 main areas (Physical, Psychological, Social, Subtle and Spiritual) that are key to achieving an overall feeling of wellness and good health.
Keep in mind that this is a bit of a shortened version, there are many more questions that can be helpful. However, this should get you started about thinking of ways to improve your own sense of health, meaning and purpose.
Technorati tags: wellness, health survey,
Hunger and Memory
It’s always a good idea to see how new findings fit in with previous knowledge, and also to see if they make sense. We have previously met the hormone leptin, which is involved in decreasing appetite. Its twin is the hormone ghrelin. Discovered in 1999, ghrelin comes from some of the cells lining the stomach and acts in the hypothalamus to increase appetite. When the stomach is empty it is released into the circulation and travels to the brain where it activates receptors in many different regions. Some research has indicated that one of the reasons why gastric bypass surgery may be effective is because it reduces levels of ghrelin and therefore reduces appetite.
Research published in December 2004 showed that in healthy young men, sleep deprivation caused a decrease in leptin levels and an increase in ghrelin levels, which, as expected, was associated with an increase in hunger and appetite. This is one reason why getting less sleep than you need may cause you to gain weight.
A new study published in the journal Nature Neuroscience, has found an intriguing link between ghrelin and memory. I noticed that the BBC also picked up on this interesting story. Researchers at Yale have discovered that ghrelin acts in an ancient part of the brain known as the hippocampus: so named because it is shaped like a sea-horse. (As an amusing aside, the old German pathologists thought it looked like a silk worm, so that’s what they called it!) The hippocampus has a number of functions, but is most of all essential for learning new material.
The researchers showed that mice who lack the ghrelin gene had 25% fewer synaptic connections between their hippocampal neurons. They then did the next step, and injected normal mice with ghrelin. They promptly increased the number and density of their synaptic connections, which correlated with significant improvements in the animals’ performance on several tests of learning and memory.
So that means that a hormone produced by the stomach can control some brain functions, and this may represent a link between metabolism and the ability to learn. The more that we discover, the more we see the intimate interactions between the brain, intestines and heart.
This link makes good sense: we know that memory can be switched on and off by a range of factors. In order to help us come up with options for handling the environment and for remembering things to avoid, memory is often switched on at times of stress. Hunger is a form of stress, and it makes good biological sense that we might be more alert and better able to remember and to recall information when hungry. It stands to reason that this has enormous survival advantage. If our early ancestors had not had this hunger/memory link, they might well have died out in the competition for food.
This gives some credence to the old advice that it is best not to try to study or to take an exam on a full stomach. Just have enough food to make sure that you have ample fuel, and that you are not distracted by hunger pains.
Technorati tags: hunger, memory, stress, study habits
Satiety: Another Kind of Gut Feeling
According the World Health Organization, there are currently over one billion overweight people in the world today. The ever-increasing prevalence of obesity in young people promises that this pandemic is likely to worsen in the coming years, putting an intolerable strain on healthcare systems. I have frequently commented on the problems of using a reductionist approach to weight management. You probably know from personal experience that any diet works for a while and then, unless something drastic happens, the weight usually returns. Similarly some of the drugs available for treating obesity may indeed work, but usually only in the short term and their usefulness is limited by side effects.
I want to say more about why the problems of weight can be difficult to manage and why the solution is not another fad diet aimed at modulating one hormone, such as leptin, or one neurotransmitter like serotonin or dopamine. I have mentioned before that there are multiple systems involving at least 260 tightly interconnected hormones and chemical transmitters coordinating the control of body weight. There are so many because weight is critical to survival and, with the possible exception of the brain, the more critical a system, the larger the number of fail safes and backups: the greater the degree of redundancy. Imagine a tent being secured by 260 ropes. But not just any ropes, these are intelligent cooperative ropes. Cut one, and the tent will stay in place because there are still hundreds left in place. Give it a little time, and the remaining 259 ropes will take up the slack, and the tent remains unmoved. Professor Steve Bloom from the Hammersmith Hospital and Imperial College Faculty of Medicine in London, has been a world leader in research into intestinal hormones and weight management for over thirty years, and he has just published a brief overview that focuses on just a few of the hormones known to be involved in the maintenance of body weight, and highlights the reason why some of them are attracting the interest of pharmaceutical companies. As well as holistically-oriented physicians.
It is now known that the regulation of appetite and food intake involves a complex series of interactions between higher cognitive centers in the brain, more primitive brain regions that we share with birds and reptiles, and the rest of the body. Amongst the key players in this whole vast orchestra are the endocrine systems of the gut, that play an important role in inducing and maintaining feelings of satiety.
The list of gut hormones involved in the maintenance of weight is a long one, that can be confusing to people who are not expert in the field. Here are just a few of them:
- Cholecystokinin
- Glucagon-like peptide 1
- Peptide YY
- Oxyntomodulin
- Ghrelin
- Pancreatic polypeptide
This is by no means the whole list, but you get the idea. At least one model for obesity suggests a breakdown or deficiency of some of the gut hormones that normally signal satiety. In effect, people do not know when they are full. In addition, disturbances of some of these hormones may lead to fat being deposited in some of the danger areas of the body, particularly inside the abdomen.
If I were to give you a breakdown of all the recognized weight control systems in the brain, I think that both of us would probably fall asleep
Yes, these understandings will enable drug manufacturers to produce new drugs to help with obesity. But that is only part of the story. We have found time and again, that the most effective way to normalize weight and eating habits is to deal with it from five different directions:
- Physical
- Psychological
- Social
- Subtle
- Spiritual
In previous articles I have already given some broad brush strokes about what constitutes healthy eating. Strategies that work WITH rather than against systems that have been evolving for millions of years. In future articles I shall also share some of the weight management techniques that I detail in my book Healing, Meaning and Purpose.
Technorati tags: satiety, weight loss, weight control, diet, holistic diet, healthy eating






