Rethinking Cancer
Over the last thirty years, there has been a gradual change in the way in which we conceptualize biological processes. Although the lion’s share of research is still dedicated to biochemical processes involving DNA, RNA and the cell membrane, other important concepts are being quite widely accepted. They include:
- Fetal imprinting
- Epigenetic control
- Self-organization
- Self-regulation
- Coherence over time
- Information exchange with the environment
- Symbiosis
- Morphogenesis
One way of thinking about this is to describe cells, organs and bodies as coherent information-rich processes. And when things go wrong, it is because these processes have gone awry. Information medicine is designed to bring the system back into coherence and harmony.
I have spoken before Integrated Medicine and in the next posting I am going to talk more about the difference between Integrated, integrative and integral medicine. But at this point suffice to say that Integrated Medicine is information medicine based on an understanding of these principles.
Several years ago I presented a paper at a closed meeting where I introduced the term “adult dysmorphogenesis,” to describe the way in which some disease processes – such as arteriosclerosis, arthritis and Alzheimer’s disease – could be better understood not as degenerative conditions, but as deranged information systems. These in turn disrupted the normal self-organizing principles of the body that lead it to constantly correct and repair itself. Part of my reasoning was that we were constantly seeing apparently irreversible conditions like broken down joints being repaired by information medicines like acupuncture and homeopathy.
With that background I was very interested to read an important paper in the journal Theoretical Biology and Medical Modelling.
The paper begins by highlighting three odd observations:
- Throughout the animal kingdom cancer hardly ever occurs in tissues that have a strong ability to regenerate
- In animals in which cancer occurs frequently, its incidence rises with age. If it occurs in a young animal it usually occurs in a tissue that has already been damaged
- In animals that have a strong ability to regenerate and repair organs, these mechanisms remain fairly efficient throughout life. In animals with weak regenerative and repair mechanisms, they tend to become less efficient with age.
The authors propose that when an organ is damaged it receives a signal to start undertaking repairs. The cancer cell is the one cell in an organ that is able to respond to the signal telling it to start to proliferate. It is the one cell that is trying to restore function. So simply removing a cancer might not work if the organ remains damaged: new tumor cells would simply keep emerging.
This paper is a good complement to another in the same journal. This one is a bit more mathematical, but also views cancer as a dynamic systems problem.
Ideas like this have come and gone before, but I have not seen them so well presented before, and they open up some new ways of thinking about a set of problems that is altogether too common.
Moving away from thinking that cancers are all simply the result of mutated or messed up DNA toward the idea that they may owe just as much to the environment in which they grow makes very good sense.
Spicy Foods as Cancer Killers

Several news services have picked up a very important piece of research in the February 16th issue of the journal Biochemical and Biophysical Research Communications.
In a nutshell, they have shown that capsaicin, an ingredient of jalapeno peppers, triggers cancer cell death by attacking mitochondria, the energy producing organelles in the cell. Some of the reports were a little confused and confusing and also missed out some critical pieces.
So first, a bit of revision, this is a graphical representation of what a mitochondrion looks like:
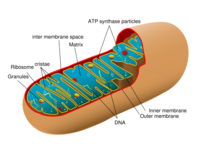
The mitochondrion is the primary producer of energy in the cell, converting molecules derived from food or stores into adenosine triphosphate (ATP) and several other less important molecules. ATP is the energy “currency” throughout the body. In recent years we have discovered that there are a number of diseases that are a result of faulty mitochondrial metabolism.
One of the biggest problems about most forms of chemotherapy for cancer is that the treatments often damage normal cells as well as the malignant ones. Therefore a great deal of research has aimed at identifying differences between normal and malignant cells.
Over the last ten years, increasing evidence has shown that mitochondrial dysfunction is a key feature of many types of cancer as well as part of normal aging. This has lead to the idea that we might have a new therapeutic target if cancer cell mitochondria are different from those in normal cells.
This new study showed that the family of molecules to which capsaicin belongs, the vanilloids, bind to proteins in the cancer cell mitochondria to trigger apoptosis – programmed cell death – without harming surrounding healthy cells. Capsaicin was tested on cultures of human lung and pancreatic cancer cells.
As the lead researcher Timothy Bates has said, “We believe that we have in effect discovered a fundamental ‘Achilles heel‘ for all cancers.”
This is extraordinarily interesting, not least because capsaicin is already in use for the topical treatment of peripheral neuropathy and some inflammatory conditions of the skin including psoriasis. The amount of capsaicin used in the experiments was similar to amounts that could probably be ingested safely. So now the next step if to see whether these observations can be translated into a viable treatment option for cancer, and if so, which types.
What the research does not say is that eating a lot of spicy food will help prevent or treat cancer.
The reports that I have seen have failed to mention that one of the reasons for doing this research was that some spices have been used in traditional Chinese and Indian medicine for many centuries for the treatment of several conditions, and some of the investigators are engaged in the Nottingham UK–China Collaboration on Complementary and Alternative Medicine.
How many more treasures are waiting for us in the archives of traditional medicine?
And how many have already been lost as plant and animal species become extinct?
Reducing Your Cancer Risk
“The doctor of the future will give no medicine, but will interest his patients in the care of the human frame, in diet, and in the cause and prevention of disease.”
— Thomas Alva Edison (American Inventor, 1847-1931)
I am sure that you will agree that prevention is better than cure. And this is a good time of the year to review where you are in your life and what you want or need to do for yourself and your loved ones.
According to a study reported in the Lancet in November 2005 more than one third of cancer deaths are attributable to nine modifiable risk factors.
To evaluate exposure to risk factors and relative risk by age, sex, and region, the investigators analyzed data from the Comparative Risk Assessment project and from new sources, and they applied population-attributable fractions for individual and multiple risk factors to site-specific cancer mortality provided by the World Health Organization.
Of the seven million deaths from cancer worldwide in 2001, approximately 2.43 million (35%) were attributable to nine potentially modifiable risk factors. Of these deaths, 0.76 million were in high-income and 1.67 million in low- and middle-income nations; 1.6 million were in men and 0.83 million deaths were in women.
Smoking, alcohol use, and low consumption of fruits and vegetables were the leading risk factors for death from cancer worldwide and in low- and middle-income countries. In low- and middle-income regions, Europe and Central Asia had the highest proportion (39%) of deaths from cancer attributable to the nine risk factors studied.
For women in low- and middle-income countries, sexual transmission of human papilloma virus (HPV) was also the leading risk factor for cervical cancer. Smoking, alcohol use, and overweight and obesity were the most important causes of cancer in high-income countries.
Between 1990 and 2001 mortality from cancer decreased by 17% in those aged 30 to 69 years and rose by 0.4% in those older than 70 years, according to the authors, but this decline was lower than the decline in mortality rates from cardiovascular disease for men and women. The decline in mortality in men was largely due to reduction in mortality from lung, prostate, and colorectal cancers, while in women, lung cancer increased in the 1990s, and death rates for breast and colorectal cancer decreased. An article published almost ten years ago in the journal Cancer Epidemiology, Biomarkers, and Prevention, it was estimated the worldwide attributable risk for cancer to infectious agents as 16%.
The nine factors were:
- High body mass index
- Low fruit and vegetable intake
- Physical inactivity
- Smoking
- Alcohol abuse
- Unsafe sex
- Urban air pollution
- Indoor use of solid fuels
- Injections from healthcare settings contaminated with hepatitis B or C virus
This all makes good sense, but it is good to see high quality research in reputable journals confirming what we suspected. The research also gives us further compelling reasons for taking a good look at our lifestyles and hopefully the motivation to do something to improve them. And in the case of air pollution and injection of contaminated products, to be active in getting things cleaned up.
“Keep your own house and its surroundings pure and clean. This hygiene will keep you healthy and benefit your worldly life.”
— Sathya Sai Baba (Indian Spiritual Teacher, c.1926-)
“Length of life does not depend so much on a good physical constitution as it does on the best use of the six non natural things, which if we rule aright, we shall live long and healthy lives: to divide the day properly between sleep and waking; to adjust our air to the needs of the body; to take more or less food and drink according to our age, our temperament and whether we live an active or inactive life; to take exercise or rest according to the quantity of food and whether we are lean or fat; to know ourselves and be able to rule our emotions and subject them to our reason. Whoever handles these wisely will live long and seldom need a doctor.”
–Giorgio Bagliivi (Italian Physician, Pathologist, Researcher and Author of De Fibra Motrice, 1669-1707)
“The best doctor prevents illness, a mediocre one treats illnesses that are about to occur, and an unskilled one treats current illnesses.”
–Chinese Proverb
Hormone Replacement Therapy, Breast Cancer and Causality
It seems a remarkable "coincidence" that they very day after writing about breast cancer screening, we should hear the news about a sudden fall in the rates of breast cancer amongst a certain proportion of the population.
Researchers from the M.D. Anderson Cancer center in Houston presented their data at a meeting of the San Antonio Breast Cancer Symposium. They recorded a 7% drop in new breast cancer cases in the US in 2003, ad an even bigger fall – 12% – in cases of hormone-dependent breast cancer among women aged 50-69. This is the first time that breast can cancer rates have fallen since 1945.
The decrease was most striking for women with so-called estrogen-positive tumors, which account for 70% of all breast cancers. It is the growth of these tumors that may be fueled by estrogen.
The scientists believe that the fall could be linked to the fact that millions of women gave up hormone replacement therapy (HRT) following reports questioning its safety. Around 14,000 fewer US women were diagnosed with breast cancer in 2003, compared with the previous year. The number of American women on HRT had halved by the end of 2002 in the wake of a large study was halted in 2002 after evidence emerged indicating that the therapy was associated with an increased risk of developing breast cancer.
The data are striking, but they need to be confirmed. That being said, there was a different type of study in last month’s issue of the Journal of Clinical Oncology. Researchers found an even larger drop in breast cancers in some parts of the State of California where there had been some of the highest rates of HRT use in the nation.
If the figures are correct – and they will have to confirmed – they could be explained by existing tumors stopping growing, shrinking or disappearing so that they could not be detected.
When I was a full time endocrinologist I saw a great many women who suffered terribly with menopausal symptoms, but I always declined to use HRT because of my take on the research data. I used dozens of alternatives, and if they failed, I had plenty of colleagues who were happy to use HRT, but I was always uneasy about using it.
There is also another important point: epidemiology can never prove causality. We have a plausible link, but no direct proof that a fall in the use of HRT is responsible for the fall in breast cancer.
Let me give you another example. Few people doubt the link between cigarette smoking and lung cancer, but no causality has ever been proven. Typhoid can cause a horrible illness, but all that the epidemiologist can do is to suggest an association between the bug and the pattern of an outbreak. It requires a microbiologist to prove that the bacterium Salmonella Typhi is the cause of the symptoms.
A number of years ago I became involved with the Oxford Causality project. It was fascinating, because not only did we call into question the issue of uni-causality in medicine – one cause for one illness – but some scientists and philosophers – such as Roy Bhaskar and Rom Harre even went so far as to suggest that “laws” of nature are better thought of as “habits” of nature. Clearly there are laws and there is causality. I throw a stone into a pond and there should be a plopping noise and then the ripples spread out. If there were no laws, then atoms could disintegrate. But at the deepest levels of nature, it no longer appears that we live in a clockwork universe in which free will is an illusion.
This is not just of theoretical importance, I recently received some interesting correspondence after I mad some comments about how self-cutting, if ignored, could lead to the development of borderline personality disorder. One correspondent thought that this implied causality, but I do not think so. “Disorders” are best viewed as deviations from a norm and they usually appear in bits and pieces. For example, some people with bipolar disorder may have had problems years before the illness had declared itself. The first signs were there, but they could have evolved along a dozen different pathways. Some people with borderline personality disorder have had varying degrees of distress since childhood, but back then it was impossible to say for sure what was wrong.
It is usually a mistake to try to find one cause for a problem. It is equally a mistake to try and diagnose a problem prematurely. We sometimes need to wait and see how things will evolve.
Screening for Breast Cancer
An important report came out in the middle of October that doesn’t seem to have been reported in much detail by the mainstream media in the United States.
It concerns screening for breast cancer. This is a most important issue: breast cancer is the most common form of malignancy in women and it carries a high morbidity and mortality. Though there can be a genetic component, there are also a number of important environmental factors. Some of those for which there is decent evidence include:
- Circulating levels of estrogens and androgens
- Late first pregnancy
- Having no children
- Not breast-feding
- Alcohol consumption
- Post-menopausal weight gain
- Exposure to artificial light
There is an array of other potential risk factors, but the point is that with so many potential risk factors, it is difficult to idenify everyone at high risk of developing the disease.
Therefore mass screening for breast cancer has been the accepted practice for many years now, and it has undoubtedly saved many lives.
But the new research – a review of studies covering half a million women – raises some important questions for women as well as clinicians.
The investigators found that for every 2,000 women who had mammograms, one would have their life prolonged but 10 would have unnecessary treatment due to false positive tests and over-dagnosis.
Dr. Peter Gozsche the director of the Nordic Cochrane Center, who led the research, said that the new research indicated that many women were being treated for slow-growing tumors that might never have affected them if they had not been picked up during the screening.
There remains no question that screening does save lives, but the new research indicates that – if it is replicated – we need to re-think the risk/benefit ratio about screening and the actions that we take if screening turns up an abnormality.
But it also should not scare people away from being screened.
It is also a good reminder that there are many potentially modifiable risk factors for breast cancer, and that is the best place to direct your attention.
Integrated Medicine and Cancer
There’s a very interesting and important piece of research from the School of Social Work at the University of South Florida in Tampa.
The title of the paper is “Patient-physician communication regarding use of complementary therapies during cancer treatment,” and it discusses something with which I’ve been very involved for many years.
The paper uses the terms “complementary and alternative medicine,” though the same principles apply to the far more sophisticated and comprehensive approaches of Integrated Medicine.
Studies from the United Kingdom, Germany, Holland, France and the United States have estimated that as many as 80% of adult cancer patients use at least one form of Complementary and Alternative Medicine (CAM) during or after conventional treatment. I’ve discussed before the pitfalls of trying to use unorthodox medicine in place of conventional medicine. In Europe some of the practices of Integrated Medicine, particularly acupuncture, homeopathy and massage, are used to help people cope with the rigors of chemotherapy and radiation therapy, rather than to treat the tumors themselves. Many people claim that they can use homeopathy or some herbal remedies as the sole treatment for different types of cancer. But I won’t endorse them unless they can show me some data.
We already know that patients frequently do not tell their oncologists about their use of unorthodox medicines and physicians consistently underestimate the numbers of their patients using them. The purpose of this study was to assess newly diagnosed cancer patients’ and oncologists’ communications with regard to unorthodox medicines. They looked at people with two types of cancer: 106 had breast cancer and 82 had prostate cancer. All the patients in the study were receiving regular conventional medical treatment.
In line with previous research, 84% reported that they were using at least one unorthodox therapy. The most popular were exercise, vitamins, prayer, and nutritional supplements.
But here was the surprise for the investigators: The oncologists surveyed were generally enthusiastic and supportive of patients’ use of these therapies. In addition to those therapies popular with patients, at least half the physicians supported massage, journal writing, support groups, acupuncture, biofeedback, and art therapy.
This was no surprise to me at all. I spent most of my clinical career in tertiary referral centers, and I’ve worked with the best of the best. The vast majority was extremely supportive of anything that would help. Every one of them was a skeptic who would say, “show me.” But once they had been shown, they would be very helpful. After all, who doesn’t want to help people get better?
It has always been so noticeable that the biggest critics, not skeptics, but critics, have been people who were less secure. Often not the “Best of the best,” they would carp and complain that “we don’t do things that way,” and “I don’t see how it could work, so I’m sure that it doesn’t.”
What this new piece of research showed was that discussions the use of unorthodox medicine were relatively rare and were most likely to be initiated by the patients. When the topic was discussed, both patients and doctors said that it usually enhanced their relationship.
What do I take away from this study?
If you, a friend or loved one has cancer, or any other type of illness for that matter, consider using something else in addition to your regular medical care. Not as a replacement, but in addition. The regular treatment will be helping the physical side of the illness, but you also need help with the psychological, social, subtle and spiritual aspects of what is going on in your life.
And guess what? Chances are that if you have a good oncologist, or any other type of conventional clinician working with you, he or she will probably be very supportive of anything that you do.
I once said at a very large meeting that if I needed to put a bone through my nose and do a dance to get someone better, I’d do it.
And I’m not the only one.
What Integrated Medicine does is to put all the cards on the table from the very beginning. We tell people that we are going to be helping guide them toward physical, psychological, social, subtle and spiritual health. They need to be able to derive meaning and purpose from what’s happened to them, rather than just cussing at their misfortune.
And then using the experience to grow as individuals and to help others.
The Integrated Practitioner will also be working with the way in which this person’s challenge is changing them. If a practitioner is not changed by the person in front of him or her, they are working only as a technician and not as a healer.
There’s nothing wrong with that, but everyone needs to be clear about what the practitioner is bringing to the table, and what their expectation is for the person who has come to see them with a problem.
For now, if you are not working with an Integrated Practitioner, do tell your health care provider if your are doing something else to help yourself.
Chances are that he or she will be very supportive.
Prostate Cancer, Shift Work and Vitamin D
One out of six American men will develop prostate cancer and more than a third of them will experience a recurrence after undergoing treatment, putting them at high risk to die of the disease.
A study from Japan in this month’s issue of the American Journal of Epidemiology, reports prospective research that examined the association between shift work and the risk of prostate cancer incidence among 14,052 working men. Compared with day workers, people who worked rotating shifts were significantly at risk for prostate cancer whereas fixed-night work was associated with a small and non-significant increase in risk. This report is the first to reveal a significant relation between rotating-shift work and prostate cancer. Previous research has found that shift work may be linked to an increased risk of breast and colon cancer.
It’s important not to jump off the deep end: we are long way from saying that sleep disturbance is linked to prostate cancer. But it is another piece of evidence suggesting a link between environmental factors and genes, since there are a number of genes that may increase a man’s risk for prostate cancer.
However, there have now been several reports that disturbances in normal body rhythms might be linked to some cancers and this report adds to that evidence. It has never been shown that the actual sleep disturbance itself is responsible for the slight increase in risk seen in these studies. It could also be that people with abnormal sleep patterns are more likely to be doing something else, for instance smoking or eating junk food that would interfere with sleep and increase people’s cancer risk.
But here’s something to think about: shift workers have been found to have reduced secretion of the sleep-inducing hormone melatonin. Melatonin has also been shown in some studies to have some potential anti-cancer effects. The studies are controversial and certainly not conclusive, despite what one or two melatonin manufacturers may say. But something that is true is that reduced secretion of melatonin has been linked to increased production of sex hormones, which play a role in regulating prostate tissues.
Under normal circumstances, secretion of the hormone is low during daytime, increases soon after the onset of darkness, peaks in the middle of the night, and gradually falls until morning. In shift workers the melatonin cycle becomes disrupted.
There has been some recent evidence that maintaining adequate levels of vitamin D may reduce a man’s risk of prostate cancer.
Another study, this time on pancreatic cancer and led by Northwestern University in Illinois has indicated that taking the US Recommended Daily Allowance (RDA) of vitamin D (400 IU/day) reduces the risk of pancreatic cancer by 43%. It is published in this month’s issue of Cancer Epidemiology Biomarkers & Prevention. This does not mean that we should start taking vitamin D supplements to reduce our cancer risk. But it ties in with research indicating that some exposure to sunlight might actually reduce the risk of some cancers. But all things in moderation: malignant melanoma and basal cell carcinoma of the skin have been increasing with increased exposure to sunlight.
Aging, Skin and Cancer
There’s a very interesting paper in this month’s issue of the journal Developmental Cell, based on research conducted at the Oregon Health & Science University in Portland, Baylor College of Medicine in Houston and Leiden in the Netherlands.
The investigators have found a pathway through which a gene’s over-expression causes stem cells in the skin to switch from creating hair follicles to creating sebaceous glands. This discovery may not only provide us with new ways of treating hair loss and oily skin, but it may help us to prevent and treat some cancers.
Skin cells turn over very quickly: just think how fast a graze gets covered over. Epidermal stem cells give rise to the outer layer of the skin that serves as a barrier for the body, as well as generating the follicles that produce hairs and sebaceous glands. These glands produce oils to lubricate the skin. In aged skin, a protein called Smad7 is overproduced, which triggers hair loss and sebaceous gland growth.
This is the first study definitively to link Smad7 over-expression and the pathological changes that occur in aged skin.
Here’s the twist: Smad7 shuts down signaling of another group of genes called Wnt. It binds to a Wnt signaling protein known as Beta-catenin and degrades it with an enzyme called Smurf2. (I don’t known why they decided to call it’s call it Smurf: it looks like ponderous chemical humor to me!) Wnt signaling is critical for organ development, but if Wnt signaling is too active, it also causes cancer.
Enhanced Beta-catenin signaling contributes to many types of cancer, including colon, lung and brain. Perhaps inducing over-expression of Smad7 or delivery of Smad7 directly to tumor cells would provide a therapeutic approach because of the boost in Beta-catenin degradation.
And finally, impaired Beta-catenin signaling contributes to neurodegeneration, such as that found in Alzheimer’s and Parkinson’s diseases, retinal degeneration, some bone density defects and aging. For these diseases, blocking Smad7-mediated Beta-catenin degradation may offer a therapeutic approach.






