Testing for Diabetes in Children
Diabetes mellitus can be a devastating illness, especially when it comes on suddenly in a child or adolescent. In young people it is usually so-called Type 1, or insulin-dependent diabetes, an autoimmune disease in which the immune system attacks the insulin-producing beta cells in the pancreas. The disease can have a major impact on the whole family, and sometimes people forget the way in which it can affect siblings whose needs often need to be subordinated to the needs of the newly diagnosed young person.
And here is an important point: even when it appears suddenly, the disease process may have been going on for some time before the clinical symptoms appear. By the time that blood glucose levels begin to rise, it usually implies that the damage to the insulin-producing cells in the pancreas has reached a critical point, and the chance of recovery is low. Anything that we can do to prevent the disease from progressing to the point of producing symptoms would be immensely helpful, and that starts with early recognition before the pancreatic damage has reached critical.
Although we now understand a great deal about the interplay of genetic, environmental and immunological factors that may lead to the illness, this knowledge has so far not helped us very much. There has been a tremendous need to try and identify the early stages of the disease, but that goal has been elusive.
In a study published in the Journal of Immunology researchers from the University of Queensland’s Diamantina Institute for Cancer, Immunology and Metabolic Medicine, are developing a simple test that may predict whether a child will develop Type 1 diabetes. They have identified a cellular pathway known as NF-kappa B that is activated in certain blood cells – monocytes and dendritic cells – of people with Type 1 diabetes.
In healthy people monocytes remain quiescent unless they are activated by an infection or other stressor. Then the NF-kappa B pathway gets activated.
In people with Type 1 diabetes things work the other way round: monocyte NF-kappa B was already activated in the blood, and when exposed to infection the pathway shut down. This tells us that there is a problem of immune control that may cause diabetes to develop in children. It is this monocyte abnormality that will hopefully form the basis of a diagnostic test.
This work is assuming more urgency since there are several trials of diabetes vaccines underway, and if successful, it may become possible to identify and intervene in children at risk of Type 1 diabetes before it occurs.
In addition, understanding why the immune system loses control before the disease starts should open up a number of new options for prevention and treatment.
Judah Folkman R.I.P.

I just heard that Judah Folkman just passed away at the age of 74. That is a name that is not widely known outside the scientific world, although a couple of years ago an excellent book –Dr. Folkman’s War – was written about him and his work.
His major work and his enduring legacy was in the field of angiogenesis: the production of new blood vessels. In the 1960s he came up with the idea that a way to kill tumors was to starve them of the blood supply that they need to survive. He was initially ridiculed, but history is now proving him correct. I got to know him twenty years ago after publishing a paper in which I described the discovery of a growth factor that is involved in the production of new blood vessels at the back of the eye in people with diabetes. Judah was very supportive and we had many good discussions about the potential role of angiogenesis not only in tumors and diabetic retinopathy, but also in diseases like rheumatoid arthritis and psoriasis.
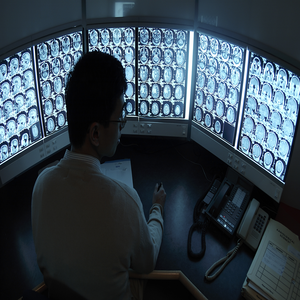
Last November, at the 12th Annual Society for Neuro-Oncology Meeting in Dallas, researchers from the University of Virginia and several other leading brain tumor centers in the United States presented data on the successful use of an inhibitor of angiogenesis in the treatment of glioblastoma multiforme (GBM), the most common form of primary brain cancer. It is hard to treat, and if it recurred after surgery, radiation and/or chemotherapy there was often not much to be done.
Building on Judah’s work, they wanted to see if they could inhibit vascular endothelial growth factor (VEGF) that has an important role in the disease. VEGF fosters the growth of a tumor by
stimulating the growth of new blood vessels to feed it. According to earlier studies, bevacizumab (BV) (Avastatin), a humanized monoclonal antibody that specifically targets VEGF, in combination with irinotecan (also called CPT-11) could have a role in recurrent glioblastoma multiforme. The researcher was an attempt to establish the clinical benefit of BV, both alone and in combination with CPT-11, in a multicenter, randomized phase II trial.
The results were very promising, substantially exceeded the pre-specified thresholds set for this work.
They looked at 6-month progression-free survival (PFS) defined as no clinical or MRI tumor growth and the objective response rate (ORR), which measures tumor shrinkage. Secondary endpoints included safety and survival. Response assessments were conducted by an independent radiographic facility that did not know which patients had been treated. All patients were followed for 24 weeks to determine efficacy and safety.
When taking BV, 35.6 percent of patients on average had a 6-month survival with no progression of their cancer, and an objective response rate of 21.2 percent on average.
The combination of BV and CPT was even more effective, with results of 51 percent and 34.1 percent, respectively.
The investigator group found similar results when they evaluated the patients. Those results showed that 44.7 percent of patients on average had a 6-month survival with no progression of their cancer, and an objective response rate of 38.8 percent on average. The combination therapy yielded results of 60.9 percent and 46.3 percent, respectively.
The surviving patients have remained in the study and are still being treated and followed, so we shall be seeing some longer-term results in the future.
In the United States bevacizumab has already been approved for the treatment of metastatic colon cancer and most forms of metastatic non-small cell lung cancer.
This is very encouraging research and a fitting tribute to a genuine medical pioneer.
More Genes Involved in Obesity

I am impressed by the progress being made by some of my former colleagues who are busily unraveling the complex genetics of obesity.
In a paper in the journal Science a group of British scientists including Chris Ponting of the Medical Research Council Functional Genetics Unit in Oxford and Stephen O’Rahilly’s group at the University of Cambridge, has made a second breakthrough in twelve months in understanding how a gene triggers weight gain in some individuals. In May we looked at the first piece of work on the gene called “FTO.”
At that time we learned that variations in the FTO gene influence people’s risk of becoming obese. This particular gene was of great interest because the genetic variant in FTO that predisposes to obesity is very common in the population.
About half the British population carries a copy of the variant and they are on average 3-4 pounds heaver than those who do not have it. The 16 per cent of the population who carry two copies of the variant and are on average 6-7 pounds heavier. We also learned that carriers of the variant have an increased risk of diabetes. However the function of FTO was completely unknown.
The new paper shows that the FTO gene codes for an enzyme – 2-Oxoglutarate-Dependent Nucleic Acid Demethylase – that can act directly on DNA. This strongly suggests that FTO might have a role in controlling how and when genes are turned on and off.
The investigators also found that FTO is highly expressed in the hypothalamic region of the brain, which has important roles in the control of hunger and satiety. In certain areas of the hypothalamus, the levels of FTO are influenced by feeding and fasting.
This is a remarkable finding. That a gene involved in obesity and diabetes has a direct effect on DNA in specific regions of the brain is very exciting. It suggests that the gene is involved in influencing how well the brain senses hunger and fullness. Small molecules derived from metabolism can modulate the activity of FTO, so we can see a direct link form food to metabolism to DNA in the brain.
The findings raise all kinds of treatment possibilities and also confirm something that I have been teaching for three decades: weight control does not start with a diet. It starts between the ears. Until you have been shown how to re-program your brain, thoughts and emotions, your chance of successfully controlling your weight is, ahem, slim.
The Evolving Obesity Pandemic
Here is something that is not too much of a shock. At least it isn’t until you look at the numbers.
People are getting heavier throughout the world, with the possible exception of south and east Asia. These are the conclusions of a one-day global “snapshot:” a single day in 2006 when doctors and nurses in 63 countries across five continents – not even including the United States – found that between half and two-thirds of men and women in were overweight or obese.
The study is being published in the journal Circulation and included 168,159 people. The initial results were published http://eurheartjsupp.oxfordjournals.org/cgi/content/abstract/8/suppl_B/B26 last year in the European Heart Journal, but this new report puts more “flesh” on the original report.
The International Day for the Evaluation of Obesity (IDEA) study looked at two measures of fatness – waist circumference and body mass index or BMI.
A BMI (weight in kg divided by square of height in meters) of 18.5 to 25 is considered healthy. A BMI over 25 is considered overweight and greater than 30 is obese. I shall have something to say about BMI in a moment.
In Eastern Asia 7% were obese, compared with:
- 36% of people in Canada
- 38% of women in Middle Eastern countries
- 40% in South Africa
Canada and South Africa led in the percentage of overweight people, with an average BMI of 29 among both men and women in Canada and 29 among South African women.
In Northern Europe men had an average BMI of 27 and women 26. In other words they were just into the overweight “category.” In southern Europe, the average BMI was 28. In Australia BMI for men was 28 and 27.5 for women. In Latin America the average BMI was just under 28.
Waist circumference was also high – 56% of men and 71% of women carried too much weight around their middle.
The overall frequency of heart disease was 16% in men and 13% in women. In Eastern European men, many of whom still smoke, the rates of heart disease, 27%, and women, 24%. By comparison in Canada the rate of heart disease in women was 8%, and in men 16%.
The rates of diabetes varied across regions. Overall, 13% of men and 11% of women were diagnosed with diabetes.
This means that the rest of the world is catching up with the United States, long considered the country with the worst weight problem.
An estimated two-thirds of Americans are overweight and a third of these are obese. In the US, the lifetime risk of developing diabetes, is also high – 33% for men and 38% for women.
In studies like these, a BMI over 25 is considered to be overweight and greater than 30 is obese. I have commented before about the limitations of using BMI, but it remains a way of getting an overall picture of what is happening in the body.
The findings are deeply worrying.
It is well known that increasing weight, particularly the amount of fat carried inside the abdomen – not the “lovers’ handles!” – increase the risk of coronary artery disease, Type II diabetes and other diseases including some cancers. That point about the “intra-abdominal” fat I all important. For years we have been told that even small increases in weight can do us harm, but that is not completely accurate. It is where the fat is deposited, not only how much we have. It is only when people become extremely obese all over that the risks of many diseases begin to climb.
The moral of the story?
Watch you the size of your abdomen, and stay tuned as I give you more advice about the Whole Person ways to control you weight.
Dopamine, Drugs and Diabetes
We recently talked about the increasing evidence that insulin has many extremely important roles in the brain.
New research by investigators at the Center for Molecular Neuroscience and the Institute of Imaging Science at Vanderbilt University Medical Center researchers, working with colleagues in Texas, has found that insulin levels affect the brain’s dopamine systems. These systems are involved in motivation, reward, salience, movement and emotional processing. Disturbances in dopamine pathways have been implicated in substance abuse, as well as schizophrenia, bipolar disorder and attention deficit hyperactivity disorder (ADHD). Drugs that interfere with the dopamine pathways may produce Parkinsonism as well as elevations of the hormone prolactin.
The psychostimulant drugs amphetamine and cocaine, as well as related medications for ADHD, block the reuptake of the neurotransmitter dopamine by dopamine transporters (DATs) thereby increasing the level of dopamine signaling. Some of these compounds also cause a massive surge of dopamine through DATs, resulting in high levels of synaptic dopamine that alter attention, increases motor activity and plays an important role in the addictive properties of psychostimulants.
The reason for examining a possible relationship between dopamine and insulin goes back to the 1970s, when it was reported that amphetamine had no effect on diabetic animals and in the 1980s it was shown that diabetic rats did not show the usual stereotyped behaviors when given amphetamine. There were also odd reports about disturbances in the enzyme dopamine-beta-hydroxylase in experimental diabetes and changes in dopamine D1 receptors in the brains of rats with induced diabetes.
These observations lead to this new research into a possible link between insulin signaling and amphetamine action.
They used a standard a rat model of type 1 diabetes in which insulin levels are massively depleted, and then assessed the function of the dopaminergic pathway in the striatum, an area of the brain rich in dopamine.
In the absence of insulin, amphetamine-induced dopamine signaling was disrupted: dopamine release in the striatum was severely impaired and expression of DAT on the surface of the nerve terminal was significantly reduced.
The lack of the DAT protein on the plasma membrane prevents the amphetamine-induced increase in extracellular dopamine, and in turn, amphetamine fails to activate the dopamine pathways that stimulate reward, attention and movement.
The researchers then gave insulin into the brains of the diabetic animals and found that the system returns to normal, indicating that the lack of insulin in the striatum directly affected amphetamine action.
They also developed a probe for brain DAT activity using functional magnetic resonance imaging (fMRI). In normal, healthy rats with plenty of insulin, amphetamine increased neural activity in the striatum. But in diabetic animals, activity in the striatum was suppressed.
So there is a powerful interplay between dopamine neurotransmitter systems and insulin signaling mechanisms. The results are some of the first to link insulin levels and dopamine function in the brain and hold several implications for human health and disease.
We need to have another look at the effect of diabetes on the brain. We have known that people with diabetes are at increased risk of cognitive impairment and depression, and we had assumed that it was because of hypoglycemia and vascular disease. Those assumptions may have been wrong.
The findings may also be important for diseases with altered dopamine signaling, such as schizophrenia and ADHD. Insulin may have something to do with the underlying brain disturbances in ADHD. Then control of insulin levels and neuronal responses to the hormone may help determine the efficacy of psychostimulants in people with ADHD.
Every now and then you see people on psychostimulant medications who need huge doses. Perhaps their problem lies with insulin rather than dopamine.
Alzheimer’s Disease: Diabetes of the Third Kind?

Insulin may have some extremely important roles in the mind as well as the body.
Though best known for its role in promoting glucose uptake into cells, insulin has at least five hundred known functions in the human body. For many years nobody was sure whether insulin was important to the brain: neurons in the brain are unusual in that they do not need insulin to enter them. But then we discovered that insulin acts on other important metabolic processes in neurons. In the brain it also does duty as a chemical messenger and as a growth factor, and brain insulin signaling is crucial for the creation of memory. Over the years a number of theorists have suggested that some neurological and psychiatric illnesses could be a result of disturbances in insulin-related processes in the brain.
It is now beginning to look as if they may have been correct.
Some recent evidence has suggested that Alzheimer’s disease and diabetes mellitus share a number of common pathways and Alzheimer’s disease is associated with peripheral insulin resistance.
New research has been published by investigators from Northwestern University in the FASEB Journal – the journal of the Federation of American Societies for Experimental Biology – that may finally nail down the reason why insulin signaling may stop working in Alzheimer’s disease.
The research team used mature cultures of neurons from the hippocampus of the brain to study synapses – the connection between neurons – that have been implicated in learning and memory mechanisms. They wanted to examine the effect of a toxic protein, known to attack memory-forming synapses, that is called “ADDL” for “amyloid ß-derived diffusible ligand.” ADDLS are small, soluble aggregated proteins that accumulate in the earliest stages of Alzheimer’s disease. The researchers had previously found that ADDLs bind very specifically at synapses, which in turn initiates deterioration of their function, shape and composition. They now went on and studied the synapses and their insulin receptors before and after ADDLs were introduced. Regions of the nerve with normal numbers of insulin receptors have no ADDL binding, but when the ADDLs are added they remove insulin receptors from nerve cells, effectively making them insulin resistant.
And an insulin resistant neuron cannot participate in the formation of memories.
This finding implies that there is a fundamental connection between diabetes and Alzheimer’s disease, and this may in turn help us to see whether existing diabetes treatments might protect neurons from ADDLs and improve insulin signaling in people with Alzheimer’s disease.
The first type of diabetes is Type 1, a.k.a. insulin-dependent or juvenile onset. The second is Type 2, a.k.a. non-insulin-dependent diabetes. So is Alzheimer’s Type 3?
It has also been known for some time that physical exercise is one of the factors that may help reduce the chance of developing Alzheimer’s disease, and we may now have a mechanism by which it can help.
This is an extraordinarily interesting and important discovery that should lead to a whole new research angle, perhaps with medicines that are already available.
It's Not the Food, It's the Size of the Plate

I grew up in a culture where the aftermath of the Great Depression and the Second World War meant that every child was expected to eat everything on their plates. That created a bit of a problem when I first moved to the United States: my conditioning led me to try and eat every morsel of those huge American portions. Fortunately I quickly noticed the impact on my waistline.
I love simple but practical and important experiments. I have just read about some very nice research from the University of Calgary in Alberta, Canada that fits the bill. It appears that simply using plates and cereal bowls with markers for proper portion sizes can help obese patients with diabetes lose weight. As a result, some can even decrease their use of glucose-controlling medications, according to a report in the Archives of Internal Medicine.
Between 1960 and 2000, the proportion of U.S. adults who were obese increased from 13.4% to 30.9%. There is clearly an association between type 2 diabetes and obesity although it is not quite as simple as saying that obesity causes diabetes, at least not until the obesity becomes extreme. But we have known for half a century that calorie restriction may improve blood sugar control in diabetics, partially by contributing to weight loss.
The enormous increase in obesity has closely paralleled the explosion of portion sizes of both food and soft drinks.
The researchers conducted a six-month controlled trial of commercially available portion control plates and bowls in 2004. The plates were divided into sections for carbohydrates, proteins, cheese and sauce, with the rest left open for vegetables. The sections approximately totaled an 800-calorie meal for men and a 650-calorie meal for women. The cereal bowl was designed to allow a 200-calorie meal of cereal and milk. The subjects consisted of 130 obese patients with diabetes with an average age 56, half of whom were randomly assigned to use the plate for their largest meal and the bowl when they ate cereal for breakfast. The other half of the participants received usual care, which consisted of dietary assessment and teaching by dieticians.
At the end of the six-months, 122 patients remained in the study. Individuals using the portion-control dishes lost an average of 1.8 percent of their body weight, while those receiving usual care lost an average of 0.1 percent. A significantly larger proportion of those using the dishes – 16.9 percent vs. 4.6 percent – lost at least 5 percent of their body weight.
In addition, at the end of the six months, 26.2% needed a decrease in their diabetes medications compared with 10.8% in the control group.
These results are important: a 5% weight loss has been shown to be clinically significant in terms of decreasing morbidity and mortality associated with obesity-linked disorders.
Simple, straightforward and very practical.
Try it!
T’ai Ch Ch’uan and Your Feet

One of the worries about getting older is that aging can adversely affect our balance and increases the chance that we can slip and fall. This is even more of a problem in people with loss of sensation in the soles of the feet due to diabetic peripheral neuropathy and other diseases. T’ai Chi Ch’uan has previously been shown to improve balance in healthy elderly adults.
A new study from the Biomedical Engineering Program, Milwaukee School of Engineering, Milwaukee, Wisconsin was just published in the journal Diabetes Technology and Therapeutics.
The aim of the study was to see if T’ai Chi improved both balance and sensory perception in the soles of the feet in healthy elderly adults and elderly adults with diabetes and sensory loss in the feet. Eighteen elderly people with a mean age of 73.1 years were tested for sensation and balance before t’ai chi training and again after 6 months of weekly sessions. Participants were grouped by their initial scores on tests of sensory perception, in order to calculate the effects of t’ai chi on sensory perception.
Plantar (soles of feet) sensation results showed that all the participants showed significant improvement in sensory ability with the 6 months of t’ai chi training. All groups also had a general improvement in all balance measures, with the greatest improvement seen in those subjects with large sensory losses. Hemoglobin A1c measurements – a standard way of estimating control of blood glucose – also decreased as a result of the intervention.
The study was small, but the effectiveness of t’ai chi training as a method of improving plantar sensation and balance in elderly adults with sensory loss, with and without diabetes, was impressive.
Another one of those things that is supposed to be impossible!
Diabetes, Inflammation and the Heart

One of the most worrying signs in people with type 1 diabetes is damage to the nerves supplying the heart. This is called cardiovascular autonomic neuropathy, and one of its first signs is a reduction in the normal heart rate variability (HRV).
It has been known for many years that people with both type 1 and type 2 diabetes have low grade inflammation, and inflammation can have profound effects on the activity of the autonomic nervous system.
A study from Sabadell in Spain has tried to sort out these links in a study of 120 people with longstanding type 1 diabetes.
They measured a great many things including tumor necrosis factor, alpha-receptors 1 and 2, IL-6, and C-reactive protein; insulin resistance and HRV in response to deep breathing and the Valsalva maneuver” forcibly exhaling against with mouth and nose closed.
They did indeed find a link between low-grade inflammation and early alterations in the nerve supply to the heart.
This is important information: when we proposed that inflammation might be an important player in diabetes back in the 1980s, it was greeted with disbelief. Twenty years on it looks as if we might have a whole new line of treatment on the horizon, which will include nutrition and exercise as well as supplements and medications.
T’ai Chi Ch’uan and Diabetic Health

Regular readers will know that I am a great fan of t’ai chi ch’uan and qigong. I have been recommending them to people for years and even taught it for a while.
I have also been very interested in metabolic problems, particularly insulin resistance and diabetes.
So I was intrigued to see a study from Taiwan that was just sent to me.
The trial involved thirty-two people with type 2 diabetes mellitus who participated in three hour-long tai chi sessions once a week for 12 weeks. The conclusions were that practicing t’ai chi might help improve one component of immune function and also improve the control of blood glucose.
The researchers found statistically significant reductions in levels of glycosylated (glycated) hemoglobin in the blood of participants, indicating improved long-term blood glucose control. Glycosylated hemoglobin or HbA1c reflects the average blood glucose over the last 8-12 weeks, implying that the improvement must have been quite swift.
They also found increased numbers of regulatory and killer T cells. This may be important: people with diabetes are at considerably increased risk of getting infections.
It is even more impressive that the study was published in the journal Diabetes Care, that is known for its exacting standards.
If you or a loved one has diabetes, you may want to think about taking up t’ai chi.
Good luck!






